Snap! Crackle! and Pop!
As we get older our knees start to make noises they have never done before.
Is this normal?
Should I be worried?
What about that strange knee pain every time I drive my car or go up and down the stairs?
The knee is the longest and most complex joint in our body.1
With so many structures surrounding it and three different joints that work together to create stability and movement, the knee is a structure very susceptible to injury; especially in any kind of contact sport.

Fig 1. Types of knee injuries.
Let’s explore the basic anatomy of the knee and the possible mechanisms that can damage these structures with elite personal trainer Jazz Alessi, a Knee Injury Specialist in London.
In this article.
I will focus on the prevention of injuries and understanding the correct rehabilitation process if already injured.
Remember, pain is not normal even as we age.
An exercise specialist can help you live a happier pain free life.
Fast facts on Knee Anatomy
- The knee is the largest and most complex joint in the body.1,2
- Flexion and extension are the two movements associated to this hinge joint.
Also, slight rotational movements are possible when it is semi-flexed.1
- It includes two different articulations: the union of the femur and tibia (tibiofemoral joint) and the union of the patella and the femur (patellofemoral joint).1,2
- The primary reason why humans can stand on two feet, compared to most other primates, is because the knees are able to extend and “lock” in this position.1
- The kneecap or patella is the largest sesamoid bone which means it is floating and does not directly connect with other bones around it.1
- The quadriceps muscle is essential in allowing humans to stand up.
The kneecap is embedded in its tendon at the lower part of this muscle.
Although one of the strongest muscles in our body, the patella is essential in reducing the energy and force needed from the quadriceps to extend the knees.1
- It is classified as a synovial joint; meaning a lot of fluid surrounds it.
This fluid is usually stored in bursae, small water balloon-like structures, that provide cushioning and reduce friction between the bones. 2,3
Knee Anatomy
Bones of the knee.
Bones: The knee is composed of three bones.
In the thigh, the femur, longest and strongest bone in the body,articulatesits upper part with the pelvis to create the hip joint and at the bottom with the patella (patellofemoral joint) and tibia (tibiofemoral joint) to create the knee.4
The patella is located in the front; embedded in the quadriceps tendon.
It protects the bottom aspect of the femur and maximises the mechanical advantages of the quadriceps muscle by lengthening it.
Therefore, less force from the quadriceps is needed to fully extend the knee.
It articulates with the femur through a grove created between the femoral condyles; allowing it to slide up or down when flexing or extending the knee.3,4
The tibia is the main bone of the inside area of the shin.
Its larger upper end, which articulates with the femur, provides a better weight-bearing surface and distribution of the weight and forces of the leg when moving.3,4
Lastly, the fibula is a thin bone located on the outer side of the shin and does not bear any weight.
Although not considered part of the knee joint, a lot of soft tissue structures related to its function attach to it.3,4
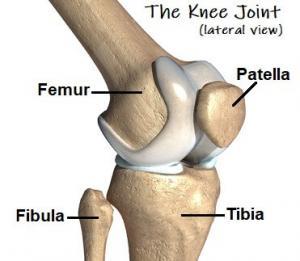
Fig 2. The knee bones.
Meniscus and Cartilage of The Knee
Cartilage:In the knee, there are fibrous cartilaginous structures in the tibial plateau (top of the bone) called menisci.
Each knee has two menisci:
- a medial meniscus located on the inside part of the tibial plateau and
- a lateral meniscus located on the outside.
These structures are some of the most important primary stabilisers and weight transmitters of the knee acting as shock absorbers that redistribute contact forces to the tibiofemoral joint and reducing friction within the joint.5,6,7
Fig 3. Ligaments of the knee. Anterior Cruciate Ligament (ACT), Posterior Cruciate Ligament (PCL), Lateral Collateral Ligament (LCL) and Medial Collateral Ligament (MCL).
Ligaments: As you can see in the picture I attached above, four ligaments join the femur and the tibia together and limit their movement.8
The Anterior Cruciate Ligament (ACL) is the most commonly known ligament and accounts for almost 40% of knee injuries in sports.
It is located in the centre of the knee and controls the rotation and forward movement of the tibia in regard to the femur.8,9
The Posterior Cruciate Ligament (PCL) is also located in the center of the joint and has an opposite function from the ACL by controlling the backward movement of the tibia in regard to the femur.9,10
Finally, the Medial Crossed Ligament (MCL) located on the inside of the knee provides stability to the inner knee while the Lateral Crossed Ligament (LCL) located on the outside of the knee and stabilises the outside.
Among other things these restrict the knee from caving in or out during movements.9,10
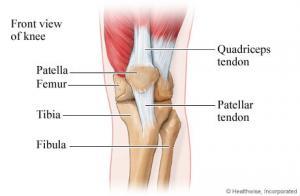
Fig 4. Tendons of the knee.
Tendons:As you can see in the picture I attached above, the knee has two main tendons that connect muscles with bones.
The quadriceps muscle located in the front of the thigh ends in a strong, thick tendon that embeds the patella called the Quadriceps Tendon.
Some fibres end at the patella while other continue down the leg merging with the Patellar Tendon and inserting themselves in the tibial tuberosity.11,12
These tendinous structures articulate the patella with the tibia and are often referred to as the extensor mechanism of the leg as they facilitate the extension of the leg powered by the quadriceps.11,12
Muscles: On the front of the thigh,the quadriceps are one of the main muscles composed of four different heads or sections:
- the vastus lateralis,
- vastus medialis,
- vastus intermedius, and
- the rectus femoris.
The rectus femoris originates in the pelvis (hip bone) and is the most superficial on the thigh, covering all three vastus and ending in the same tendon in the patella.13
On the back side of the thigh and shin, we can find the hamstrings and gastrocnemius.
The hamstring muscle is composed of three heads:
- semimembranosus,
- semitendinosus and
- biceps femoris, which extend the hip (all but the biceps femoris) and flex the knee.13,14
The gastrocnemius is a two-headed muscle that originates in the back of the femoral condyles and covers the back of the shin.
Along with the hamstrings and other muscles it works to ensure that your knee and leg performs well. 13,14
Brief movement analysis
Although the knee acts as a hinge allowing us to bend and extend,there is a slight rotation of the tibia that occurs when the knee is flexed.
If the knee is semi-flexed and the foot is off the ground, the tibia can rotate or turn to the inside and the outside.
If the foot is on the ground when the knee is flexed however, this rotation happens from the femur and not the tibia.11
Common Knee Injuries
Sprains and strains: Sprains and strains are the most common knee injury diagnosed in Emergency Rooms at about 42% regardless of the cause.
The rehabilitation process and return to activity on these depend on the severity of the injured tissues. 15, 16, 17
In sprains, ligaments are stretched beyond their normal tolerance usually during sudden or sharp rotational movements or blunt trauma to the knee that makes it cave in or out.
Strains affect muscle fibres or tendons causing tears.
Strains are commonly associated with a sudden increase in physical activity or weight load that exceeds what the body is used to.15,16,18
ACL tear: As mentioned previously, the ACL is one of the most commonly injured structures in the knee; especially in female athletes.
According to the American Academy of Orthopaedic Surgeons, about 70 % of ACL injuries in athletes happen through mechanisms such as:
- pivoting,
- cutting,
- sidestepping,
- out of control play or awkward landings, while about
- 30 percent occur from contact with other players8,9,10
An ACL tear happens when the ligament is extended past its stretching point and ruptures.
Since there are so many structures knee that work together to maintain stability and allow movement, ACL injuries are oftentimes accompanied by injuries to other ligaments (usually the MCL), meniscus and tissues.17
PCL tear: The PCL is stronger than the ACL which is one of the reasons why it is not as commonly injured.
Sports like football, basketball, American football and rugby have the highest incidence in PCL injuries.
Normally, it occurs from a direct hit to the shinbone, as would happen in a car accident, or a fall onto the leg with the foot pointing down.16,17
With an isolated PCL injury, people do not complain of feeling instability as they normally do when the ACL is torn.
For this reason, a non-surgical approach which includes physiotherapy and rehabilitation exercise is often recommended on isolated PCL tears.16
Meniscus tear: Tearing of the meniscus can occur in any age group usually from forceful twisting of the knee while planted on the ground (bearing weight).
Also, it can occur during squatting or hyperflexion of the knee, after jumping and landing with a flexed knee or from twisting as the foot hits an obstacle (like a hole, rock or uneven surface).16,18
The most common symptoms experienced include a popping sound when twisting followed by swelling and a “locked knee” that is hard to straighten.
If the rupture is large enough a piece of torn meniscus can get trapped between the femur and tibia making it impossible for the knee to extend and requiring surgery to “unlock”it.16,18,19
Meniscus tears can have long term effects on the health of the knee joint.
Since the menisci are designed to bear weight and cushion to prevent bone to bone contact, its erosion can lead to the development of osteoarthritis.18,19
Paellofemoral syndrome: Patellofemoral pain syndrome is a very common problem in adolescents and active young adults.
It occurs when nerves sense pain in the soft tissues such as tendons, the fat pad beneath the patella and bone around the kneecap.20
Similarly, it can be caused when the patella moves through the grove between the condyles.
When the knee is bent, the patella is pushed out to one side of the groove which may cause increased pressure between the back of the patella and the femur, irritating soft tissues.21
Fracture: A knee facture usually refers to the breaking of the patella due to blunt trauma or a hard fall.
Since the patella is a small bone, the pieces normally move away from their original location making surgery the best option to repair it.
This is a serious injury since the patella is fundamental when extending the knee and keeping it locked in place when extended (for example when standing up).22
Overuse: Overuse injuries to the knee can be very painful and hard to treat.
They often begin with muscular strains that can progressively worsen if left untreated.
When inflammation is present in the knee from excessive use, the surrounding structures start to rub against each other increasing the inflammation and pain.
Untreated overuse of the knee can lead to osteoarthritis which results in pain and permanent, irreparable erosion to the bone and soft tissue surrounding it.21,22
Knee rehabilitation: Ways to speed up a knee injury recovery
Whether you are recovering from a knee injury or preparing for surgery to recover from one, there are many ways to speed up the recovery process and have a more successful outcome.
# Use Myofascial Release
When the body experiences trauma or inflammation, the flexibility of the fascia, a web-like tissue that provides structure and stability, decreases leading to myofascial restrictions.
These manifest as pain, limitation of movement and decreased range of motion.
Learning and frequently using techniques to release those myofascial restrictions, such as using a foam roller, can prevent the appearance of muscular pain and stiffness after exercising as well as short and long-term movement limitations.23

Fig 5. Quadriceps Muscle Myofascial Release with Foam Roller.
# Stretch to Improve Range of Motion
Stretching is crucial to any exercise routine.
Before exercising, stretching serves as a warm-up for the muscles and tissues that will be used.
After exercising, stretching can help relieve some of the soreness associated to the activities performed.
It is important to use dynamic stretches and mobility exercises
before a workout rather than static stretches as these have been proven to decrease performance due to muscle fibre fatigue.24
Fig 6. Hamstring and calf muscle stretches.

# Improve Joint Strength
A knee injury rehabilitation programme must not only focus on a strong lower extremity but on all other areas that allow us to move while standing.
Most ACL and knee injury recovery programmes will focus on strength exercises for the quadriceps; one of the most affected structures. Likewise, they will target areas like the core and back since these are necessary for good stability when dynamically moving standing up.5,6,7
# Create Knee Stability
Patients that have suffered a sprain or tear in any ligament of the knee will often be exposed to a feeling of instability or “weakness”.
When an athlete is to return to play, stability plays a very important role in reducing the changes of re-injury.
Patients with untreated instabilities, such as an ACL injury, are more likely to end up having meniscal surgery and other cartilage damage because of the misalignment of the bones.10
# Knee Exercises Personalisation Requirements
As a rehabilitation specialist and personal trainer in London, I can help you stay strong, fit and healthy while progressively and safely increase your activity level to achieve a successful surgery and recovery.
The use of a brace, crutches or cast after an injury can impact the whole body with short and long-term repercussions.
An individualised rehabilitation knee exercise programme is essential in the recovery of any injury since it’s based on the specific goals and needs of each person.
Whether you are an athlete who wishes to continue playing, suffered a car accident or have chronic knee pain, no exercise routine should ever be the same.
ACL Reconstruction Rehab
After an ACL injury, 98% of surgeons would recommend surgery to repair the damage not only to that ligament but to surrounding structures; especially if a patient wishes to return to sport.
The rehabilitation process for an ACL injury varies according to the:
- severity of the structures damaged,
- type of surgery performed,
- physical fitness age and
- gender among other variables and a successful ACL rehabilitation can take anywhere from six to twelve months to recover.10,25,26
An ACL injury is characterised by instability; described as a feeling that the knee will “give out” at any moment.
Since the primary stabiliser is torn it is important to avoid activities like twisting, turning on jumping before and for some time after the surgery.
Likewise, a loss of quadriceps strength is one of the most common long-term symptoms that has been documented to continue even two years after surgery.10,25, 26
When preparing for surgery, it is important to wait until the swelling has decreased and the person recovers the full range of motion.
This process can take up to three weeks after the injury.
If a full range of motion is not present before the surgery, the recovery will be more difficult.25
An elite personal trainer and a specialised rehabilitation professional can provide a customised knee exercise programme aiming to strengthen key muscles, recover all functionally impaired structures and obtain symmetrical and full range of motion.
Also, they will provide you with customised stretches to help you maintain mobility and recommend some activities such as light swimming or cycling.26
Exercise is essential after surgery and can usually start as soon as two days after surgery and continue up to three or four months afterwards.
Likewise, you will be encouraged to gradually return to your normal level of activity within the first 6 weeks of the surgery and continue avoiding some movements or exercises for up to 6 months post-surgery while the graft heals correctly.25,26
Have you experienced an ACL injury and are unsure on how to start your rehabilitation process?
Let a knee rehabilitation specialist help you take your first steps into an optimal recovery.
Contact us for a FREE CONSULTATION.
What is a PCL (Posterior Cruciate Ligament) Injury?
The PCL is the ligament in charge of limiting the backwards movement of the lower leg in relation to the upper leg.
These injuries can range from simple overstretches or sprains and to complete ruptures that require a surgical approach.10,26
The most common symptoms of PCL injuries include mild knee swelling and pain in the back of the knee that worsens when kneeling.
Also, there might be instability when walking or standing and possible limitation of motion.
Given that the symptoms are not as severe as when other structures are damages, an athlete might not come in for a physician visit until a few weeks have passed from the injury and the symptoms are still present or worsen.8,9,26
Isolated PCL injuries that do not result in full rupture are usually not related to serious instability as they are with the ACL.
A full PCL rupture is usually associated with a very traumatic injury such as hitting the dashboard with the shin during a car accident or a hard fall with a flexed knee which results in damage of multiple structures simultaneously.26
Are you an athlete with pain, swelling and difficulty when trying to slow down while running? Have you been diagnosed with a PCL injury and feel unsure on how to start your recovery?
Contact us for a FREE CONSULTATION.
Conclusion:
The knee is one of the most perplexing and intricate structures in the human body. Because of this, it is also very susceptible to many types of injuries ranging from simple sprains and strainsto more complex ligament ruptures and fractures requiring surgical interventions.
A knee injury sounds like a life changing event, but it doesn’t have to be.
With the appropriate treatment tools such as myofascial release, stretching and strengthening, most can be resolved with full, successful recoveries. Customised knee rehabilitation programmes are particularly important in athletes since in 90% of the cases can lead to return to play.
Although a highly complex joint, the knee structures just like the rest of the body can recover with the proper tools but most importantly under the supervision and guidance of a trained rehab specialist.
With a limited time availability I offer you a comprehensive knee injury assessment and I will design for you the best evidence-based knee rehabilitation exercise programme which will help you to recover successfully.
If you have any questions or concerns about the advanced knee rehabilitation class, please contact Jazz Alessi on t: 020 3633 2299 (Monday – Fri: 6:30am to 9pm – Saturday: 8am to 3pm).
Request for FREE CONSULTATION here https://www.personaltrainingmaster.co.uk/contactme/
For more information on knee conditions, rehab procedures and services offered at our website, please visit https://www.personaltrainingmaster.co.uk
References:
- Cowan, H., Fascinating facts about the knee – Reader’s Digest. https://www.readersdigest.co.uk/health/health-conditions/fascinating-facts-about-the-knee
- Capital Ortho. Fast Facts on Knee Anatomy. https://www.capitalortho.com/fast-facts-on-knee-anatomy/
- Funiciello, M., What Is a Bursa? https://www.arthritis-health.com/types/bursitis/what-bursa
- Schoen, D.C., Adult Orthopaedic Nursing. Chapter 10: The Knee and the Lower Leg. Lippincott, Philadelphia, Pa.
- International Cartilage Regeneration and Joint Preservation Society (ICRS), What is Cartilage? https://cartilage.org/patient/about-cartilage/what-is-cartilage/
- Beaufils, P., Verdonk, R. The meniscus. Springer Verlag, Heidelberg.
- Slightham, C., Nall, R., Meniscus Tear of the Knee: Causes, Symptoms, and Diagnosis. https://www.healthline.com/health/meniscus-tears
- What Are Ligaments?https://www.webmd.com/pain-management/ligaments-types-injuries
- Knee ligament surgery https://www.nhs.uk/conditions/knee-ligament-surgery/
- Stanford Health Care. Types of Knee Ligaments. https://stanfordhealthcare.org/medical-conditions/bones-joints-and-muscles/knee-ligament-injury/types.html
- An Overview of Knee Pain https://www.webmd.com/pain-management/knee-pain/knee-pain-overview
- Palastanga, N., Soames, R. Anatomy and human movement: structure and functio Churchill Livingstone, Edinburgh; New York.
- Healthline Medical Network. Quadriceps Anatomy, Function & Origin https://www.healthline.com/human-body-maps/quadriceps
- What are the Hamstrings? https://corewalking.com/what-are-the-hamstrings/
- Gray, A.M., Buford, W.L. Incidence of Patients with Knee Strain and Sprain Occurring at Sports or Recreation Venues and Presenting to United States Emergency Departments. https://doi.org/10.4085/1062-6050-50.11.06
- Resnik, A.M., Resnik, J.Y. A knee and shoulder handbook: for all of us. New Haven, CT.
- Harvard Health. Knee Sprain. https://www.health.harvard.edu/a_to_z/knee-sprain-a-to-z
- NYU Langone Health. Types of Knee Sprains, Strains & Tears https://nyulangone.org/conditions/knee-sprains-strains-tears/types
- van de Graaf, V.A., Noorduyn, J.C.A., Willigenburg, N.W., Butter, I.K., de Gast, A., Mol, B.W., Saris, D.B.F., Twisk, J.W.R., Poolman, R.W., Effect of Early Surgery vs Physical Therapy on Knee Function Among Patients with Nonobstructive Meniscal Tears: The ESCAPE Randomized Clinical Trial. https://doi.org/10.1001/jama.2018.13308
- American Academy of Orthopaedic Surgeons. Patellofemoral Pain Syndrome https://www.orthoinfo.org/en/diseases–conditions/patellofemoral-pain-syndrome/
- Chevidikunnan, M.F., Al Saif, A., Gaowgzeh, R.A., Mamdouh, K.A., 2016. Effectiveness of core muscle strengthening for improving pain and dynamic balance among female patients with patellofemoral pain syndrome. J Phys Ther Sci 28, 1518–1523. https://doi.org/10.1589/jpts.28.1518
- American Association of Orthopaedic Surgeons. Patellar Fractures (Broken Kneecap) https://www.orthoinfo.org/en/diseases–conditions/patellar-kneecap-fractures/
- Ferguson, L.W., Gerwin, R., Clinical mastery in the treatment of myofascial pain. Lippincott Williams & Wilkins, Philadelphia.
- , Static Stretching and Performance. https://www.nsca.com/education/articles/kinetic-select/static-stretching-and-performance/
- Beaumont Orthopedics,ACL Tears Signs, Diagnostics, and Treatments.https://www.beaumont.org/conditions/acl-tears
- Failla, M.J., Arundale, A.J.H., Logerstedt, D.S., Snyder-Mackler, L.Controversies in Knee Rehabilitation. https://doi.org/10.1016/j.csm.2014.12.008
- Harvard Health., Posterior Cruciate Ligament (PCL) Injuries. https://www.health.harvard.edu/a_to_z/posterior-cruciate-ligament-pcl-injuries-a-to-z



