Are you under 50 years of age and have pain around the knee cap for more than three months?
You may be having patellofemoral pain syndrome (PFPS).
No reason to feel daunted!
Contact us now, here.
A focused knee injury rehabilitation program could help you to get rid of the knee pain and rehabilitate your knee in just 10 – 16 weeks.
Nicknamed as the “Movie Goer’s knee”, it is often noticed after sitting for a long time at the movies.
As the pain comes from under or around the knee cap, patients often put their palm over the knee to indicate the area of pain – the “circle sign”.
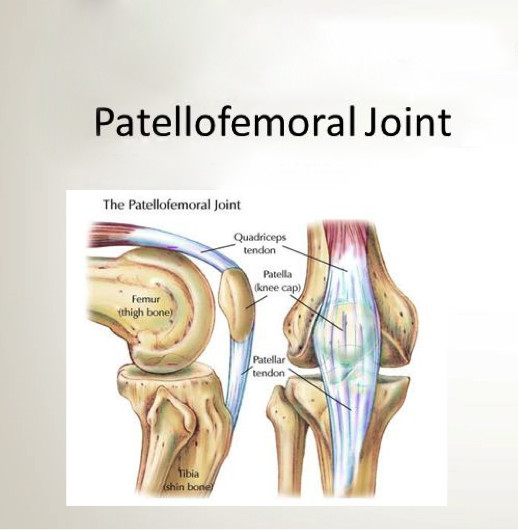
Patellofemoral pain syndrome is a group of symptoms resulting from increased pressure between the patella (knee cap) and the lower end of femur (thigh bone).
It occurs due to repeated loading, quite different from chondromalacia patellae (the cartilage under the patella deteriorates and softens – runner knee).(1)
The latter occurs as a result of damage to the cartilage on the underside of the patella.
Commonly referred to as Runner’s knee, the condition is an overuse injury occurring in young athletes especially runners.(15)Since symptoms are similar to PFPS, the two are often used interchangeably.
8 Symptoms that may indicate Patellofemoral pain syndrome (PFPS)
It is more a diagnosis by elimination.
This means, if you have not sustained any direct injury to the bone, ligament, tendon, cartilage or meniscus, it is probably patellofemoral pain syndrome.
You may recall doing a sudden burst of activity like running or climbing stairs, before the pain began.
PFPS occurs more due to sudden and prolonged overloading of the joint.
Incorrect movement of the knee cap coupled with constant pressure while bending the knee, irritates the undersurface of the knee cap.
This leads to anterior knee pain.
The clinician will also eliminate other causes such as Patellar tendinitis, Sinding Larsen Johnson or Osgood Schlater’s disease before making the diagnosis. (1,2)
Patellar tendinitis also presents with anterior knee pain (just below the knee cap) which aggravates after jumping.
Basketball players are more prone to this condition.
Sudden contraction of the quadriceps during take-off and landing puts a lot of strain on the patellar tendon, attached just below the knee cap.(17)
Sinding Larsen Johansson disease is frequently seen in adolescent athletes who have had a sudden growth spurt.
There is inflammation of the lowest point of the knee cap because of the pull of the patellar tendon. (16)
Osgood Schlatter’s disease is another condition seen in young athletes with sudden increase in height.
The patellar tendon pulls on its bony attachment on the shin bone (tibial tuberosity).
There is often a lump seen at the site of tendon attachment on the shin bone.(18)
The PFPS on the other hand is more commonly seen in older adults, military recruits, runners, bikers and cyclists.
Repeated bending of the knee, increases the stresses on the underside of the patella, causing pain.
Overweight and obese people suffer more as their joints are overloaded.(10)
The usual complaints include:
- Gradual onset knee pain with no immediate history of injury
- Vague annoying pain emanating from under or around the knee cap
- Pain while ascending/descending stairs
- Pain on cycling or running
- Pain after prolonged sitting or squatting
- Feeling of instability and clicking or popping sound
- Pain on contracting the quads (bulky muscle on the front of thigh)
- Clarke’s sign positive (forceful contraction of the quadriceps, while pressing the knee cap down causes sharp pain)
Do you have any of these knee injury signs?
- Contact now HERE – the knee rehab trainer specialist for your comprehensive FREE CONSULTATION. If you have a knee diagnosis Jazz will carry out a comprehensive fitness knee rehab assessment providing you with a customised knee exercise programme to avoid re-injury and knee pain, rehabilitating your knee and return to more happiness, good life and excellent fitness.
8 top causes for patellofemoral pain syndrome (PFPS):
- Certain sports or professions: PFPS constitutes 18-25% of the cases visiting the sports injury clinic.
Cyclists, long distance runners, football players are most affected.(10)
Repeated bending presses the different areas of patella to the femur.
This irritates the nerve endings causing pain.
Around 15% of military recruits are affected by PFPS for the same reason. (10)
- Change in training surface or intensity– Training on a hard surface can increase the impact on the entire leg. Similarly, increasing the running mileage can also put excessive loads on the knee.
- Gender: Females are at a greater risk as compared to males due to the difference in their lower limb and pelvis alignment.
Though still under debate, a wider pelvis, is thought to increase the angle of pull of the quadriceps muscle (Q angle).
This may abnormally stress the patella while walking or running.
- Muscle weakness: As the trunk and legs are connected at the pelvis, any weakness of the abs and hip muscles will disturb the alignment of the knee.
Increased low back arch, causes increased quadriceps activity which presses the knee cap into the femur.(8)
Similarly, weakness in hip abductors and external rotators (muscles that move the thigh out), causes the knee to fall inwards while jumping or running.(5)
This makes the knee unstable.
Quadriceps has to contract more to stabilise the knee, increasing the pressure on the knee cap.
- Abnormal patellar movements: The patella moves through an arc as the knee bends and straightens.
If the soft tissue structures (ligaments, retinaculum and IT band) are tight, they tend to limit the movement of patella.
This again results in abnormal loading of the knee.
- Patellar tilt or shift: The patella is normally positioned in the middle without tilting to either side. A high lying patella or laterally positioned patella does not move through the full range of knee movement.
This creates moments of increased loading on the patella undersurface.(12)
This is more prominent after prolonged sitting.
- Abnormal patellar groove– The patella moves through a groove present at the lower end of the femur. If this groove is shallow, the knee cap tends to slip out as the knee bends.
- Knocked knees and flat foot: Both these conditions, rotate the shin bone inwards, changing the line of force through the knee.(9)
Is my knee cap moving incorrectly? Role of patella maltracking in patellofemoral syndrome
Patella (knee cap) moves as we bend and straighten our knee.
In normal course, there is no undue friction between the patella and the lower end of femur.
The movements are full and pain free.
When the patellar position is incorrect, knee movements are affected.
There is increased contact between the surfaces causing pain while bending the knee.
What does my knee cap to move wrongly?
A number of reasons may cause the knee cap to move differently.(4)
- Lateral tilt or shift of patella
- Delayed activation of the vastus medialis
- Tight peripheral structures
- Increased Q angle
- Patella Alta (high patella)
- Mediopatellofemoral ligament insufficiency
- Shallow trochlear groove
- Infrapatellar fat pad edema
Tight or short lateral structures pull the patella outward.
A wrongly positioned patella heightens the abnormal stresses on the undersurface of patella.
Repeated loading in this situation causes pain.
Similarly, short medial ligament prevents patellar dislocation.
Its insufficiency causes the patella to dislocate repeatedly.
In addition, if the groove which lodges the patella moves is shallow, also results in recurrent dislocation especially while running.(10)
Swelling in the area above the knee cap (fat pad) also does not allow the knee cap to move fully. (11)
Not only the joint geometry, but muscle dynamics also plays a key role in proper movement of the knee cap.
A delayed activation of vastus medialis versus a stronger vastus lateralis action moves the patella out of position.
Increased Q angle also changes the path of the patella. (12)
If it is more as seen in persons with wider pelvis (women).
Are you suffering from any type of knee pain?
- Book your FREE CONSULTATION now HERE with Jazz Alessi, a knee rehab trainer specialist. Jazz will carry out a comprehensive fitness knee rehab assessment and provide you with a customised knee exercise programme to avoid re-injury and knee pain, rehabilitating your knee and return to happiness, good life and excellent fitness levels.
What not to do when you have PFPS: 13 Exercises and Habits to avoid

Everyone tells you what you can do to relieve the pain.
However, randomly done exercises can do more harm by putting more stress on the knee joint.
They can stretch or strengthen the wrong muscle group, damaging the knee further.
If you live in the city then, the knee rehabilitation exercises taught by a physiotherapist or an elite personal trainer in London are more beneficial in relieving knee pain.
In addition, some simple changes in your lifestyle can help you stop the pain in its tracks and also prevent it from coming back.
- Deep squats or squatting positions
- Cross legged sitting
- Lunges
- Walking or running uphill and down hill
- Going up and down the stairs frequently
- Kneeling or All fours position
- High impact aerobics
- Cross trainer
- Using the incline mode while doing the treadmill
- Leg presses or knee extension machines
- Wearing high heels
- Jumping
- Cycling with your seat too low
Knee Exercises: Highly recommended for patellofemoral syndrome
Research has shown physiotherapy to be extremely effective in managing patellofemoral pain syndrome.(6)
More than 90% of individuals who embark on a knee rehabilitation program get symptom free in just 6 weeks(7)although we are also different and in some cases a patella femoral syndrome and patella maltracking recovery will take longer.
Personalised knee rehabilitation exercises planned by a sports therapist or a personal trainer will not only work to relieve pain but stop it from coming back!
If you live in town once you have received clearance from your doctor or physiotherapist, one on one sessions with a rehabilitation trained elite personal trainer in London is highly recommended.
A rehab trained elite personal trainer will not take into consideration only your knee joint but also any other muscle imbalances in the entire pelvis-hip-knee-ankle-foot unit.
Remember they are interconnected and interdependent!
Furthermore, an elite personal trainer will assess your needs and match your knee strength to your challenges, goals and activity levels.
He can also work with you on any weight and nutrition issues. (19)
A session with an elite personal trainer vs a regular PT is a package deal, as you are evaluated and holistically supported to rehabilitate and heal.
The exercises are taught in the right way and progressed when you plateau.
Also, you are dramatically decreasing your injury risks!(20)
- Do you want to become healthy and fit and enjoy life at full again?
- The most rehabilitation trained and sought-after elite personal trainer in London, Jazz Alessi offers you a FREE CONSULTATION to see if we are a good fit to work with each other.
5 Exercises for Patellofemoral Pain Syndrome
- Straight leg raising: Easiest yet most effective way to strengthen quadriceps. Lie flat on your back.(2)
Tighten your quads and lift your leg approximately 6-8 inches off the floor.
Hold for 10 seconds and return to starting position.
Repeat 15 times on each leg.
- Nordic Hams Curl: Most scientific way to eccentrically strengthen the hams.
Beware the difficulty level is high.
Come into the kneeling position and anchor your legs under a strong bar.
Alternately ask someone to hold them.
With your spine in neutral, lean forward to touch the floor.
You can use your hands for support. 3 sets of 5 reps can be exhilarating.
- Hams stretch: Lie on your back. Bend hip and knee to 90 degrees.
Clasp your hands around the thigh, and straighten your knee.
The toes should point to the ceiling.
Feel the stretch in the back of thigh.
Hold for 20 seconds.
Return to starting position and repeat 3-5 times for each leg.
- IT band stretch: Stand with a support on the good (unaffected) side.
Take the affected leg behind the good leg and lean sideways towards the good side.
Till you feel a stretch in the affected thigh.
Hold for 20 seconds.
Return to starting position and repeat 3-5 times for each leg.
- Ankle Proprioception: Extremely crucial to prevent reinjury!(3)Activating receptors in the knee and ankle ensures timely activation of the hip and knee muscles and proper patellar alignment.
Begin with balancing on a wobble board with both feet.
Slowly progress to balancing with eyes closed and then to single leg balance board exercises.
Do you have a diagnosis, want to get rid of your knee pain, and would like to the best elite personal trainer in central London to support you rehabilitate your knee injury?
- Contact Now – the knee rehab specialist, elite personal trainer in central London or at your location for your comprehensive FREE CONSULTATION. Jazz will carry out a comprehensive knee rehab assessment and if you are a good fit for each other he will work alongside you providing you with the customised knee exercises to avoid re-injury, rehabilitate and return to happiness, good quality life and fitness.
References
- Petersen W, Ellermann A, Gösele-Koppenburg A, Best R, Rembitzki IV, Brüggemann GP, Liebau C. “Patellofemoral pain syndrome.” Knee Surg Sports TraumatolArthrosc. 2014 Oct;22(10):2264-74. doi: 10.1007/s00167-013-2759-6.
- Kooiker L, Van De Port IG, Weir A, Moen MH “Effects of physical therapist-guided quadriceps-strengthening exercises for the treatment of patellofemoral pain syndrome: a systematic review.” J Orthop Sports Phys Ther. 2014 Jun;44(6):391-B1. doi: 10.2519/jospt.2014.4127. Epub 2014 Apr 25.
- Rabelo ND, Lima B, Reis AC, Bley AS, Yi LC1, Fukuda TY, Costa LO, Lucareli PR. “Neuromuscular training and muscle strengthening in patients with patellofemoral pain syndrome: a protocol of randomized controlled trial. “ BMC MusculoskeletDisord.2014 May 16;15:157. doi: 10.1186/1471-2474-15-157.
- Lankhorst NE, Bierma-Zeinstra SM, van Middelkoop M. “Factors associated with patellofemoral pain syndrome: a systematic review.” Br J Sports Med. 2013 Mar;47(4):193-206. doi: 10.1136/bjsports-2011-090369. Epub 2012 Jul 19.
- Thiago R. T. Santos,Bárbara A. Oliveira, Juliana M. Ocarino, Kenneth G. Holt, and Sérgio T. Fonseca, “Effectiveness of hip muscle strengthening in patellofemoral pain syndrome patients: a systematic review” Braz J Phys Ther. 2015 May-Jun; 19(3): 167–176. Published online 2015 May 29. doi: 10.1590/bjpt-rbf.2014.0089 PMCID: PMC4518569 PMI26039034
- Rixe JA, Glick JE, Brady J, Olympia RP “A review of the management of patellofemoral pain syndrome.”, Phys Sportsmed.2013 Sep;41(3):19-28. doi:10.3810/psm.2013.09.2023.
- Clijsen R, Fuchs J, Taeymans J, “Effectiveness of exercise therapy in treatment of patients with patellofemoral pain syndrome: systematic review and meta-analysis.” Phys Ther.2014 Dec;94(12):1697-708. doi: 10.2522/ptj.20130310. Epub 2014 Jul 31.
- Yılmaz Yelvar GD, Baltacı G, BayrakcıTunay V, Atay AÖ , “The effect of postural stabilization exercises on painand function in females with patellofemoral pain syndrome.” 2015;49(2):166-74. doi: 10.3944/AOTT.2015.13.0118.
- Matsuda S, Miura H, Nagamine R, Urabe K, Hirata G, Iwamoto Y, “Effect of femoral and tibial component position on patellartracking following total knee arthroplasty: 10-year follow-up of Miller-Galante I knees.” Am J Knee Surg. 2001 Summer;14(3):152-6. https://www.ncbi.nlm.nih.gov/pubmed/11491425
- Calista M. Harbaugh, Nicole A. Wilson, and Frances T. Sheehan,” Correlating Femoral Shape with Patellar Kinematics in Patients with Patellofemoral Pain” J Orthop Res. 2010 Jul; 28(7): 865–872.doi: 1002/jor.21101
- Jibri Z, Martin D, Mansour R, Kamath S’ “The association of infrapatellar fat pad oedema with patellarmaltracking: a case-control study.” Skeletal Radiol. 2012 Aug;41(8):925-31. doi: 10.1007/s00256-011-1299-8. Epub 2011 Oct 20.
- Pal S, Draper CE, Fredericson M, Gold GE, Delp SL, Beaupre GS, Besier TF , “Patellar maltracking correlates with vastus medialis activation delay in patellofemoral pain patients.” Am J Sports Med. 2011 Mar;39(3):590-8. doi: 10.1177/0363546510384233. Epub 2010 Nov
- Alfredo Schiavone Panni, Simone Cerciello, Chiara Del Regno, Alessandro Felici, and Michele Vasso, “ Patellar resurfacing complications in total knee arthroplasty”IntOrthop. 2014 Feb; 38(2): 313–317. Published online 2013 Dec 21. doi: 10.1007/s00264-013-2244-3
- BaldonRde M, Serrão FV, Scattone Silva R, Piva SR., “Effects of functional stabilization training on pain, function, and lower extremity biomechanics in women with patellofemoralpain: a randomized clinical trial.” J Orthop Sports Phys Ther. 2014 Apr;44(4):240-A8. doi: 10.2519/jospt.2014.4940. Epub 2014 Feb 25.
- https://www.healthline.com/health/chondromalacia-patella#symptoms
- https://kidshealth.org/en/teens/slj-syndrome.html
- https://www.healthline.com/health/patellar-tendonitis
- https://patient.info/health/knee-pain-patellofemoral-pain/osgood-schlatter-disease
- https://fitness.edu.au/15-benefits-personal-trainer/
- https://www.livestrong.com/article/497395-7-benefits-of-hiring-a-personal-trainer/


