For obvious reasons, “menopause” is always mentioned in reference to women.
Most of you would have heard of a bone-related condition called “Osteoporosis” more in connection with women than men.
The UK-based medical journal ‘Lancet’ reports that osteoporosis is becoming increasingly common in women almost 10 years earlier than men and this have disastrous consequences on women health. [1]
Why so?
In my article I will help you understand this better and what you can do to safely reverse this (safe is the keyword here) but, let us first look at what “Menopause” and “Osteoporosis” are.
Osteoporosis – an “age-related” decline in bone health
Literally,
Osteoporosis means “porous bones”.
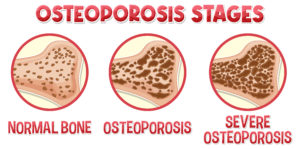
When you are young, your bones are strong and dense, so minor injuries do not pose any problem. However, as you may age, bone density decreases and your bones become more porous and brittle.
This is true for both men and women, some of whom go on to develop Osteoporosis.
As per the UK Clinical Guidelines, research shows that Osteoporosis reduces:
- bone mass,
- increases your bone fragility, and
- increases your risk of developing bone fractures.[2]
A person with Osteoporosis is more prone to bone injury and fractures, even in minor falls.
Important to note is the fact that this is a progressive condition (develops gradually) and is usually “silent” (often unrecognised until fracture).
The prevalence of Osteoporosis is increasing as life expectancy is increasing as per the Report on Osteoporosis Epidemiology in the UK. [3]
At this time, over 3 million people in the UK are affected by Osteoporosis and this number is on the rise.[4]
You would think that Osteoporosis, being age-related, would affect both men and women in equal measure.
You are wrong here, clearly, research shows women are more affected by Osteoporosis, more so if they are post-menopausal.
Stay tuned to know more about Osteoporosis prevention after menopause and if you have specific questions and want to know to reverse osteoporosis in a way that will work for your metabolism and body.
BOOK YOUR FREE CONSULTATION NOW!The link between osteoporosis and menopause
Menopause – this is a natural phase in women!
Menopause is definitely not a disease or disorder.
It occurs naturally in every woman at the end of the reproductive phase of her life.
As you approach your mid-forties, your periods become less frequent or irregular.
This phase is called “Perimenopause” and can last for a few months or even a year before your periods stop altogether.
You are considered to have attained menopause if your periods have stopped for 12 months in a row.
The age at which Menopause occurs and the symptoms experienced vary from woman to woman.
Research shows that the average age for menopause is between 45 and 55 years of age.
In the UK, research shows that the average age for a woman to reach menopause is 51.[5]
During menopause, women develop prominent symptoms like:
- hot flashes,
- night sweats,
- vaginal atrophy and dryness.
Besides these, menopause and bone health are closely related.
Osteoporosis is the most prevalent condition in menopausal women and is strongly associated with excessive risks of hip and other bone breaking and a low quality of life.
In general, women have a higher risk of osteoporosis than men.
This could be attributed to:
- women having fewer skeletons and bone mass
- pregnancy consuming a large amount of calcium and other nutrients
- the cessation of estrogen secretion by ovaries after menopause.
Did you know that…
Although with age, bone thinning occurs in both men and women, it speeds up in women during perimenopause and menopause ?
So, why do we need to explore the role of “hormones” in bone health?
Because research shows that bone loss and hormonal changes are closely related.
How osteoporosis affects bone density and strength?
Your bones are constantly changing from birth to adulthood.
There are two processes going on continuously in your body:
- bone deposition (bone building) and
- bone resorption.
During childhood and young adulthood, bone deposition is faster than bone resorption.
Peak levels of bone mass and strength are reached by age 30.
After the fourth decade of life, bone resorption speeds up while bone building declines, thus bone strength deteriorates with resultant fractures.
Unsurprisingly, research shows that there is an increased risk of osteoporosis with age.
Therefore, postmenopausal osteoporosis is increasing.
The role of hormones in bone health and Osteoporosis
To know about hormones and osteoporosis risk, let us understand the bone formation process.
Bone formation (a complex process) is governed by many hormones in the body, particularly calcium-regulating hormones.
The major mineral in bones in calcium.[6]
Eating calcium-rich food will help you have strong bones.[7]
Have plenty of green veggies, whole grains, and fortified plant-based milk in your diet.[8]
You might be surprised to know that sex hormones are also extremely important in the growth and maturation of bone, regulation of bone turnover, and maintaining the mass and strength of bone.
Androgen and bone density have a strong correlation.
Testosterone, a male hormone is important for skeletal growth through its direct effect on bone and its ability to stimulate muscle growth.[9]
That’s why men are naturally stronger (in a physical sense) than women!
Though men are stronger and research shows that levels of androgen and bone density decide the risk of osteoporosis in men.[10]
Did you know that estrogen is considered a main stimulant for calcium deposition, meaning it facilitates bone building ? [11]
Research shows that estrogens regulate your bone remodeling by modulating the production of cytokines and growth factors from bone marrow and bone cells.[12]
Estrogen is important for bone health in both men and women.
It works as a “bone protector”.
And therefore, menopause and bone health are closely related.
Menopause is the physiological result of a decline in the female productive hormones such as estrogen. During perimenopause, the amount of estrogen in your body fluctuates wildly.[13]
A fallout of the estrogen decline at menopause means that there is rapid bone loss and thinning.
Risk factors for Osteoporosis in Menopause
Bone density and menopause go hand in hand.
Estrogen deficiency in postmenopausal women is the primary contributor to osteoporosis in elderly women.
Other important risk factors for postmenopausal osteoporosis include:
- Advanced age: The risk of osteoporosis increases with the age of the woman post-menopause.
- Smoking and alcohol intake: These have been linked to an increased risk of bone fracture and osteoporosis.[14]
- Intake of non-nutritious diet: Diets deficient in Calcium and vitamin D generally result in poor bone health.
Recent UK clinical guideline for the prevention and treatment of osteoporosis has recommended having an intake of calcium (minimum 700 mg daily) preferably through diet intake or otherwise by supplementation.[15,16]
- Medical conditions and medications that affect bone health are rheumatoid arthritis, Hyperthyroidism, Hyperparathyroidism, and Diabetes mellitus.
Bone loss and hormonal changes are correlated.
Consumption of steroids and blood thinner also affects bone density.
- Osteoporosis runs in the family.
Your risk of developing osteoporosis increases if a close relative has had this condition.
Therefore, your clinician will always check your family history.
- Lifestyle factors such as diet and exercise play a key role.
Sitting for long periods of time and lack of exercise aggravate the risk of developing osteoporosis.
This recent research study by UK scientists published in 2022 in the British Journal of Sports Medicine has concluded that exercise and physical activity help improve bone strength and the risk of falls.[17]
Remember, in the case of osteoporosis weight-bearing exercises should be tailored according to your ability and need.
Therefore, you should consult a specialist personal trainer expert in osteoporosis. You could also find a great Yoga teacher and practice 1-2-1 yoga at home!
 Remember that Prevention is better than cure!
Remember that Prevention is better than cure!
Maintaining strong bones is the main preventive approach for osteoporosis, better health outcome, more happiness and enjoyable life.
Do you have a DEXa scan and it shows osteoporosis and your bones are at risks?
Are you keen to get strong bones and eliminate your bone break risks ?
BOOK YOUR FREE CONSULTATION NOW!Conclusion
Osteoporosis, a loss of bone mass and density, is a serious concern for women especially as they age.
Postmenopausal women are unique in that their health risks increase not just due to age but also due to the loss of estrogen which results into postmenopausal osteoporosis.[18]
With average lifespan extending beyond 70 years, most women will spend more than one third of their life beyond the menopause transition period.
Therefore, the health of menopausal women is a prime concern worldwide.
Based on a customised programme that covers specialist exercises, and bespoke nutrition, the osteoporosis outcome could be changed.
Helping you to move your bones safely from bone breaking risks to your best safe place takes a bit of time but, using Jazz’s specialist osteoporosis customisations and comprehensive exercise and nutrition programmes (very effective and easy to implement in practice) it can be done in about half of the time!
Keen to get started?
BOOK YOUR FREE CONSULTATION NOW!Who is Jazz Alezzi?
Jazz Alessi is the leading London’s specialist osteoporosis personal trainer who has transformed life of many women with osteoporosis thorough his customised nutritional advice and osteoporosis reversal programme in London.
He follows the most recent and up-to-date strategies laid down by UK Clinicians to design a laser-sharp rehabilitation programme based on your weight, strength, and overall health status that help you achieve your personal goals of health.
Jazz is very well aware of the scientific facts published in Systematic Review published by UK physicians about Exercise for preventing and treating osteoporosis in postmenopausal women. [19]
Discuss with Jazz for the osteoporosis reversal programme and forget about the menopause symptoms!
No matter what are your symptoms of menopause and how severe is your osteoporosis, Jazz will listen carefully to you professionally, connect the dots and understand more about your health, lifestyle, diet preferences, and goals.
Accordingly, Jazz will create a tailor-made safe and effective osteoporosis reversal programme especially for you to help you come off with flying colours.
FAQs
1. How can I prevent Osteoporosis during Menopause?
Eat a balanced nutritious diet rich in proteins, vitamins and minerals (especially Calcium). Take advice of expert nutritionist. Stay physically active, avoid alcohol and smoking. A regular habit of physical exercise is important to decrease bone loss. Practice customised strength training and weight-bearing exercises to strengthen your bones.
2. Can Menopause causse Osteoporosis?
The short answer is yes. Keeping all factors constant, a postmenopausal woman is more liable to have Osteoporosis than a man of the same age. This has to do with the fact that older men have higher levels of circulating estrogen (the hormone that protects bones) than do postmenopausal women.
3. How can I tell if I have Osteoporosis?
You may not even notice that your bones are weakening, as osteoporosis may not cause symptoms for decades. A bone fracture can be the first sign of the disease. This is why women 65 and older are urged to get the test known as DXA or DEXA (dual-energy X-ray absorptiometry), which measures bone density in the spine and hips.
4. What are the treatment options for Osteoporosis?
For women at high risk for osteoporosis, especially perimenopausal women with low bone density and other risk factors, estrogen or other therapies are available to prevent bone loss. You need to adopt lifestyle changes (balanced diet, exercising, avoiding smoking and excessive alcohol intake, strategies to reduce fall risk), along with few supplements and medications to increase bone density and to improve bone strength.
References:
1. Compston, J.E.; McClung, M.R.; Leslie, W.D. Osteoporosis. Lancet (London, England) 2019, 393, 364-376, doi:10.1016/s0140-6736(18)32112-3 https://pubmed.ncbi.nlm.nih.gov/30696576/.
2. Compston, J.; Cooper, A.; Cooper, C.; Gittoes, N.; Gregson, C.; Harvey, N.; Hope, S.; Kanis, J.A.; McCloskey, E.V.; Poole, K.E.S.; et al. UK clinical guideline for the prevention and treatment of osteoporosis. Archives of osteoporosis 2017, 12, 43, doi:10.1007/s11657-017-0324-5 https://pubmed.ncbi.nlm.nih.gov/28425085/.
3. Clynes, M.A.; Harvey, N.C.; Curtis, E.M.; Fuggle, N.R.; Dennison, E.M.; Cooper, C. The epidemiology of osteoporosis. British medical bulletin 2020, 133, 105-117, doi:10.1093/bmb/ldaa005 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7115830/.
4. Barker, K.L.; Newman, M.; Stallard, N.; Leal, J.; Minns Lowe, C.; Javaid, M.K.; Noufaily, A.; Adhikari, A.; Hughes, T.; Smith, D.J.; et al. Exercise or manual physiotherapy compared with a single session of physiotherapy for osteoporotic vertebral fracture: three-arm PROVE RCT. Health technology assessment (Winchester, England) 2019, 23, 1-318, doi:10.3310/hta23440 https://pubmed.ncbi.nlm.nih.gov/31456562/.
5. Vigneswaran, K.; Hamoda, H. Hormone replacement therapy – Current recommendations. Best practice & research. Clinical obstetrics & gynaecology 2022, 81, 8-21. , doi:10.1016/j.bpobgyn.2021.12.001 https://pubmed.ncbi.nlm.nih.gov/35000809/.
6. Vannucci, L.; Fossi, C.; Quattrini, S.; Guasti, L.; Pampaloni, B.; Gronchi, G.; Giusti, F.; Romagnoli, C.; Cianferotti, L.; Marcucci, G.; et al. Calcium Intake in Bone Health: A Focus on Calcium-Rich Mineral Waters. Nutrients 2018, 10, doi:10.3390/nu10121930 https://pubmed.ncbi.nlm.nih.gov/30563174/.
7. Cormick, G.; Belizán, J.M. Calcium Intake and Health. Nutrients 2019, 11, doi:10.3390/nu11071606 https://pubmed.ncbi.nlm.nih.gov/31311164/.
8. Muñoz-Garach, A.; García-Fontana, B.; Muñoz-Torres, M. Nutrients and Dietary Patterns Related to Osteoporosis. Nutrients 2020, 12, doi:10.3390/nu12071986 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7400143/.
9. Vingren, J.L.; Kraemer, W.J.; Ratamess, N.A.; Anderson, J.M.; Volek, J.S.; Maresh, C.M. Testosterone physiology in resistance exercise and training: the up-stream regulatory elements. Sports medicine (Auckland, N.Z.) 2010, 40, 1037-1053, doi:10.2165/11536910-000000000-00000 https://pubmed.ncbi.nlm.nih.gov/21058750/.
10. Hoppé, E.; Bouvard, B.; Royer, M.; Chappard, D.; Audran, M.; Legrand, E. Is androgen therapy indicated in men with osteoporosis? Joint bone spine 2013, 80, 459-465, doi:10.1016/j.jbspin.2013.03.002 https://pubmed.ncbi.nlm.nih.gov/23587643/.
11. Cheng, C.H.; Chen, L.R.; Chen, K.H. Osteoporosis Due to Hormone Imbalance: An Overview of the Effects of Estrogen Deficiency and Glucocorticoid Overuse on Bone Turnover. International journal of molecular sciences 2022, 23, doi:10.3390/ijms23031376 https://pubmed.ncbi.nlm.nih.gov/35163300/.
12. Pacifici, R. Estrogen, cytokines, and pathogenesis of postmenopausal osteoporosis. Journal of bone and mineral research : the official journal of the American Society for Bone and Mineral Research 1996, 11, 1043-1051, doi:10.1002/jbmr.5650110802 https://pubmed.ncbi.nlm.nih.gov/8854239/.
13. Troìa, L.; Martone, S.; Morgante, G.; Luisi, S. Management of perimenopause disorders: hormonal treatment. Gynecological endocrinology : the official journal of the International Society of Gynecological Endocrinology 2021, 37, 195-200, doi:10.1080/09513590.2020.1852544.
14. Yuan, S.; Michaëlsson, K.; Wan, Z.; Larsson, S.C. Associations of Smoking and Alcohol and Coffee Intake with Fracture and Bone Mineral Density: A Mendelian Randomization Study. Calcified tissue international 2019, 105, 582-588, doi:10.1007/s00223-019-00606-0 https://pubmed.ncbi.nlm.nih.gov/31482193/.
15. Gregson, C.L.; Armstrong, D.J.; Bowden, J.; Cooper, C.; Edwards, J.; Gittoes, N.J.L.; Harvey, N.; Kanis, J.; Leyland, S.; Low, R.; et al. UK clinical guideline for the prevention and treatment of osteoporosis. Archives of osteoporosis 2022, 17, 58, doi:10.1007/s11657-022-01061-5.
16. Lanham-New, S.A. Importance of calcium, vitamin D and vitamin K for osteoporosis prevention and treatment. The Proceedings of the Nutrition Society 2008, 67, 163-176, doi:10.1017/s0029665108007003 https://pubmed.ncbi.nlm.nih.gov/18412990/.
17. Brooke-Wavell, K.; Skelton, D.A.; Barker, K.L.; Clark, E.M.; De Biase, S.; Arnold, S.; Paskins, Z.; Robinson, K.R.; Lewis, R.M.; Tobias, J.H.; et al. Strong, steady and straight: UK consensus statement on physical activity and exercise for osteoporosis. British journal of sports medicine 2022, 56, 837-846, doi:10.1136/bjsports-2021-104634 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9304091/.
18. Cauley, J.A. Estrogen and bone health in men and women. Steroids 2015, 99, 11-15, doi:10.1016/j.steroids.2014.12.010 https://pubmed.ncbi.nlm.nih.gov/25555470/.
19. Howe, T.E.; Shea, B.; Dawson, L.J.; Downie, F.; Murray, A.; Ross, C.; Harbour, R.T.; Caldwell, L.M.; Creed, G. Exercise for preventing and treating osteoporosis in postmenopausal women. The Cochrane database of systematic reviews 2011, Cd000333, doi:10.1002/14651858.CD000333.pub2 https://pubmed.ncbi.nlm.nih.gov/21735380/.



