No pain. Definite gain!
Back pain is an extremely common occurrence in people of all ages and nationalities.
But, did you know that recent studies indicate that back pain affects 12-30% of the world population every day?1
In 2015, over half a billion people worldwide reported low back pain and more than a third of a billion reported neck pain.
These conditions were ranked the fourth leading cause of disability-adjusted life years (DALYs) globally just after:
- ischemic heart disease,
- cerebrovascular disease and
- lower respiratory infection.2
From poor posture to serious trauma, back injuries can develop due to numerous reasons.
Likewise, they can present themselves as isolated occurrences or correlate with multiple other symptoms.
Although in many cases back pain will self-resolve within a few days or weeks, it is often a reoccurring condition; making it a debilitating condition that affects:
- social,
- emotional and
- physical health.3,4
If you have suffered a lower back or neck Injury in the London area, learn about the multiple benefits of visiting a back rehabilitation professional today.

Seven Signs that you need Back Rehabilitation:
Non-specific back pain is a pretty common occurrence associated with:
- disability and
- work absenteeism worldwide.
When back pain is not associated to a specific condition such as a:
- tumour,
- spinal injury,
- osteoporosis or
- radicular syndrome among others,
It is often classified as non-specific.
Recent studies have discovered that 40% of patients with non-specific back pain will not recover on their own within three months and of these, only 40% will recover during the following 12 months.
Likewise, the recurrence is very high.5
Let’s look at seven red flags or warning signs that you should visit a back rehabilitation specialist:
1. Pain that lasts for more than a week
If you have suffered an accident, it is normal for tissues to suffer from inflammation that can last a few days or weeks.
On the contrary, if you have not experienced any kind of trauma, back pain should subside within a few days.
Back pain that appears suddenly can be related to simple causes such as poor sleeping position, strenuous exercise or a strained muscle.5
These conditions, although simple, can be very painful and uncomfortable and make us worry that something might be really wrong.
Before visiting a doctor or rehabilitation specialist, try giving your back pain a few days and use conventional methods like a:
- hot bath,
- heat pad,
- massage and
- over the counter pain medications or muscle relaxers to diminish the symptoms.
If the pain continues or worsens after a week, please check in with a doctor or health professional.6
2. Little niggles that keep coming back
Sometimes, back pain can present as a sudden, large and painful experience that knocks the wind out of you.
Other times, we experience small bouts of pain that appear to come and go.
As mentioned previously, back pain is extremely common and can be attributed to a multitude of causes.
You might experience back pain this week from a poor sleeping position and next month because you lifted something heavy.
In these situations, the site might be sore and painful for a few days but should decrease and eventually disappear with rest.
However, Did you know that chronic back pain is characterized by lasting over 12 weeks?6
This does not necessarily mean that it will hurt at the same intensity all 12 weeks or more, but rather that the pain does not seem to disappear despite rest and conventional treatments such as applying heat and using over the counter medications.
Recurrent and inexplicable back pain that seems to come and go with no apparent pattern for extended periods of time might be a sign for you to visit a doctor.
3. Referred pain, tingling and numbness
Pain is a very subjective experience.
Only you know how and where you are experiencing pain.
What can seem like the worst pain possible for one person can be moderate or mild to another.
Radiculopathy
When back pain is accompanied by other symptoms such as tingling and numbness, it could predict an underlying condition such as radiculopathy.6,7
A radiculopathy is defined as a series of symptoms associated with a pinched nerve that can include:
- pain,
- weakness and
The most common lower back radiculopathy is sciatica where the body structure, muscles and the sciatic nerve is compromised, causing pain that radiates down the leg and numbness.
In the cervical area, radiculopathies often cause tingling and numbness that spreads towards the arm, as well as weakness when lifting objects such as a cup.7
4. Back pain with fever and chills
Back pain should never be accompanied by fever and chills.
Whether the symptoms start suddenly or appear gradually, they could be indications of a more severe and life threatening illness.
Spinal infections, meningitis and other conditions are usually associated with neck or back pain.
If you experience adverse symptoms like:
- vomiting,
- fever and chills.
You could be experiencing a hidden infection.
This will require urgent medical care to assess if it is bacterial or viral and proper medication to reduce the symptoms.8
5. An accident or trauma associated with incontinence or loss of bowel control.
As explained previously, radiculopathies can be associated with back pain as they are often the result of compromised muscles balance, body structures, and pinched nerve roots or nerves.
Cauda Equina Syndrome is a radiculopathy that is associated with severe, life threatening symptoms.9
In this syndrome, the bundle of nerves at the end of the spine become damaged by trauma or other conditions.
The main symptoms of this condition include:
- back pain,
- sciatica-like numbness
- tingles down one leg,
- incontinence and in more severe cases can lead to
These can appear suddenly or gradually and can be permanent depending on the severity and the time the nerves have been compressed.
If you have been involved in an accident or have experienced trauma to your back, make sure that get medical attention promptly.
6. Pain that does not seem to improve but rather gets worse.
As mentioned previously, back pain that lasts a few days is not unusual.
If you are resting and avoiding unnecessary strain on your back, symptoms should gradually decrease and disappear.
On the contrary, back pain that seems to worsen as time passes can be a sign of a more serious illness; especially if accompanied by other symptoms.10
Many gastrointestinal or internal organ conditions cause referred pain to the back.
- kidney stones,
- gall bladder stones,
- urinary tract infections,
- prostate problems and aortic aneurysms commonly present as intense back pain that gradually worsens.
These conditions are usually accompanied by other symptoms such as:
- vomiting,
- abdominal tenderness,
- difficulty breathing or urinating.
Some of these conditions can become life threatening if unattended while other will still require medical supervision to help alleviate the symptoms.10
7. Identify and Correct the Causes of Back Pain:
As mentioned previously, back pain is a multifactorial symptom that can be associated to numerous conditions that range from simple to complex.11
Let’s explore some of the most common causes of back pain and how to identify them.
Strained Muscle
Muscle strains are the most common back injuries and occur when the muscles are stretched beyond their limit of too suddenly causing muscle fibres to overstretch or tear.
Most often, activities like lifting, twisting or bending in an unusual or forceful way cause a muscle to spasm and inflame.
Pain from a strain can range from mild to severe, worsens with activity and decreases with rest.12
Posture
It is frequently mentioned that bad posture is a cause for back pain but most modern studies now show that there is no such thing as “bad” posture.13
Posture relates to the adaptations in our muscles and joints that allow us to remain upright and functional.
Poor posture will be any position the body is exposed to for prolonged periods of time causing muscle fatigue and compensations.
Pain can change out posture, mobility and stability as the body normally avoid situations that provoke pain both consciously and unconsciously.13

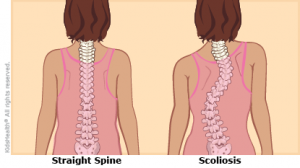
Scoliosis
Our backs are naturally curved as an ‘S’ when looking at it from the side and create a straight line when looking from the back.
Scoliosis refers to a deviation of the normal curvatures of our spine; usually to the sides.
These deviations can occur from childhood or develop through time because of postural problems.
Likewise, they can vary in severity from barely noticeable to severe compromise and deformity.
Children that develop scoliosis suffer more severe postural deviations and complications than adults who develop it.
In severe childhood cases, surgery is the best course of action.
For less severe cases or in adults suffering from scoliosis, corrective postural exercises are ideal and yield great results in alleviating pain.13
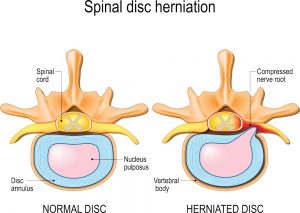
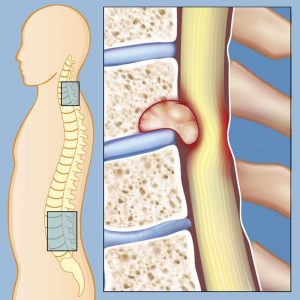
Disc Herniation
Disc herniation is a very common cause of back pain.
Our spine is composed of vertebrae (bones) that articulate with each other through discs.
These discs have a fibrous outer ring and a viscous and soft nucleus.
Repetitive trauma to the spine can cause wear and tear in the discs which can cause the outer ring to rupture and the nucleus to spill out degenerating the disc and oftentimes compressing nerve roots.
There are other factors which count and must be taken into consideration but, usually if the herniation does not compress a nerve root it might not generate back pain.
Disc hernias are most common in the lower back area, tend to worsen with improper movement and exercise and improve with rest and if compressing a nerve root aggravate when:
- sneezing and
- coughing.
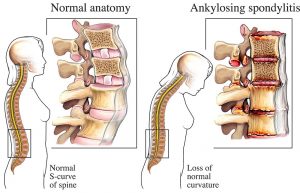
Ankylosing Spondylitis (or AS)
There are specific conditions that can create pain and stiffness to the spine.
Ankylosing Spondylitis is a condition that affects 1 in 200 adults.
Its cause has been greatly studied and has reflected a strong genetic component; with symptoms manifesting between 18 and 35 years of age. 14
AS is characterized by pain, tenderness and stiffness and some degeneration of the upper back curvature (kyphosis).
Inflammatory conditions can cause severe pain and often manifest in flare-ups followed by periods of no symptomatology.
Tumours
Tumours, both benign and cancerous, are not an uncommon occurrence in the spine.
A tumour is an overactive clump of cells that reproduce quickly and invade other areas.
In some cases, tumours can originate in the spinal area or can be the result of metastasis (the spread of cancer to other secondary locations).
The symptoms associated will depend on the size and location of the tumour and can range from pain and discomfort that is worsened by activity or at night to numbness and paralysis from spinal cord compression.
Malignant tumours, cancer, will usually be accompanied by inexplicable weight loss, loss of appetite, constant and severe pain.12
Infection
Did you know that the Spine is not immune to infections caused by bacteria or fungus that invade the spinal canal and surrounding tissues?
Infections can be deadly and often come as a post operatory complication.
Common infections include:
- meningitis,
- vertebral osteomyelitis, and
- spinal cord abscesses.
The main symptoms include:
- fever,
- chills and in some cases
- deformities to the surrounding tissues. 15
Suffering from Back Pain in London?
Living with a back injury does not have to imply living with pain.
Did you know that low back pain probably affects around one-third of the UK adult population each year?
Of these, only around 20% (1 in 15 of the population) will consult their GP about their back pain.
This results in 2.6 million people, in the UK, seeking advice about back pain from their GP each year.16
As mentioned previously not every back pain requires a visit to the doctor.
In fact, a number of the cases of back pain will self-resolve with conventional treatment:
- rest,
- avoiding unnecessary strain and
- pain management protocols (ice, heat and over the counter pain killers).
Given that in most cases the cause for back pain is not serious enough to seek treatment, most of us usually ignore it and fail to notice other important symptoms mentioned above.
Pain can become chronic; alleviating at times but never fully going away.
In fact, back pain alone accounts for 40% of sickness absence in the NHS and overall it costs £10 billion for the UK economy.17
If you are experiencing recurring back pain, you are not alone.
If you have any back injury diagnosis and clearance to exercise with a comprehensive, individualised evaluation process, I can help you find the best Back Rehabilitation Programme in the Canary Wharf area of London.
Living with frequent back pain can be a thing of the past. Contact us now for a FREE CONSULTATION by Jazz Alessi – London’s Top Back Pain Rehabilitation Specialist.
Minimise your Back Pain:
There are many alternatives to minimising the symptoms of your back pain.
Although exercise may seem like the last thing on your mind when struggling with back pain, it is important to work on maintaining flexibility, mobility and gradually, as the symptoms decrease, focus on strengthening your back with the right back rehabilitation programme.
Let’s review some of the best ways to reduce the detrimental effects of back pain in your day you day life.
Reduce the risk of other health problems and comorbidities.
Did you know that chronic diseases are oftentimes linked to back pain?18
Most adults in the world do not fulfil the daily recommendation of 30 minutes of exercise daily.
Sedentary lifestyles are predominant in cities around the globe.
This has led to an increase in chronic conditions such as heart disease, diabetes and obesity; all of which relate to chronic back pain.
The NHS states that a simple 30-minute workout every day is the best strategy to prevent many chronic conditions.
Stretching
Stretching can be very soothing if you struggle with back pain and stiffness.
If you work at an office or in front of a computer for many hours, stretch breaks are a wonderful way to relieve the symptoms of staying in the same position for a long time.
A great alternative for prolonged sitting time is to use a rolled up towel or shirt and attach it to the lower back side of the chair.
The towel will provide lumbar support and relieve back pain.
This is especially useful if you drive for long periods of time without stopping.

Exercising
When we exercise, the increase in blood flow and nutrients also increases the body’s production of different hormones like endorphins.
This chemical produced in the brain binds to an opiate receptor in the pain control system in the brain and spinal cord which decreases the perception of pain. In many ways, endorphins can mimic the effects of commonly prescribed drugs like morphine and codeine but in a natural way. This generates an overall feeling of happiness and wellbeing that lasts for a few hours.19
If you have a specific condition, certain exercises can trigger or increase your back pain.
Visiting a back rehabilitation specialist that can adequately evaluate and prescribe the best routine for you can make the difference between worsening symptoms and improvement.
Are you ready to look good and feel good?
To stop letting back pain get the best of you and get back to living your life to the fullest?
London, don’t let pain get in your way!
Get more information about our Full Body Transformation Program here.
Better Postural Habits.
As previously mentioned, the only “bad” posture is the one in which the body stays for prolonged periods of time.
Frequent stretch breaks, changing positions and keeping active are good ways to prevent poor postural habits.
A great alternative for the office space is alternative sitting such as:
- exercise balls,
- standing desks or even
- treadmill and stationary bicycle desks.
Although at a higher cost than regular desk chairs, these provide the possibility of moving around during the day which can also reduce:
- anxiety and
- stress.

Reduce fear of movement.
One of the biggest fears of anyone who suffers from back pain is making it worse.
This usually causes them to avoid exercise and movement even when they might not be triggering the pain or worsening the symptoms.
A customised to your needs exercise rehabilitation programme that is well designed will not cause pain which will in turn encourage everyone to continue moving as the symptoms start to disappear and the problem resolves.21
Osteopathy in London:
Osteopathy is very popular alternative in England.
In most cases, osteopaths complete 4 years of full time training and must continue their education and certification every year.22
Osteopathy is a branch of alternative medicine that uses manual mobilisations and manipulations of the muscle and bone.
For lower back pain, osteopaths can offer alternatives to reduce the symptoms associated.
Since osteopathy focuses on a holistic, fully body assessment, osteopaths will look not only for pain and tenderness in the area but also in other locations of the body.23
Looking for an exercise back pain expert that can help you transform your strength and pain?
Request for free consultation here https://www.personaltrainingmaster.co.uk/contactme/ For more information on back rehabilitation and injury rehabilitation services offered at our website, please visit https://www.personaltrainingmaster.co.uk
Best Pilates Trainer in Canary Wharf, London:
Are you experiencing back pain?
Have you visited several professionals with no real improvements?
Are you an accountant, work in the bank or a corporation or live in the Canary Wharf area of London and looking for a back rehabilitation specialist?
If you answered yes to any of the questions, I have an answer for you.
An evidence-based program
As a rehabilitation specialist I have had the opportunity of working with people with all sorts of injuries.
Personalised and thorough evaluations are the key principle to my rehabilitation services.
Every person is different and even if they struggle with similar conditions, their objectives and lifestyles can vary greatly.
Customisation and correct exercise awareness
Your training sessions will begin with an in-depth initial evaluation including all your:
- medical information,
- lifestyle
- daily activities
And a series of physical possible fitness tests (depending how you feel) to assess your current movement, exercise form, strength and structural health state etc.
Based on the results, I will create a personalised exercise routine accordingly.
Your sessions will be guided and supervised and continuous supporting you whilst live assessing will occur to determine when you are ready for progressions.24
Safe progressions
“Safety first” is a motto you will often hear me say.
Training a person efficiently requires long term expertise, rehab experience (specific) and dedication.
We are all different.
Back injuries can greatly benefit from interventions using the Pilates method in a customised manner.
So, what makes my personalised routine different from a Pilates class?
Classes are structured to allowed a variety of individuals participate but in no way do they cater to a person with a specific injury.
Sometimes they might even injure you.
Through my extensive evaluation process, I will select the best exercises to prescribe for YOU. 25
Pilates Exercises for Back Pain
A Pilates exercise programme is effective in improving:
- disability,
- pain,
- flexibility and
- balance in patients with chronic non-specific low back pain.
Depending on your back injury some of the following exercises might be used in basic Pilates sessions to improve back pain symptoms and strengthen the muscles associated.
Make sure that before trying any of these exercises you obtain clearance from your medical doctor.
Pelvic Tilt to Pelvic Curl:
The Pelvic Tilt and Curl are the base for the correct activation of the core muscles during more complex exercises.
Have you heard of the bridge exercise before?
Mastering the pelvic tilt and curl will teach you how to properly activate the core muscles in order to protect you back from injury.
To perform the Pelvic Tilt and Curl lay face up on the floor with your legs flat.
Bend your knees and plant your feet flat on the floor.
From this position, tuck your tail bone in, tighten your glutes and elevate them from the floor.
A great way to understand how to activate your muscles correctly is to place an exercise band around your thighs and press outwards (trying to stretch the band) as you lift your buttocks off the ground.
Your legs should not open to the sides for this exercise, but pushing against the band will help you understand what muscles should be active when doing so.
Understanding the slight movement of the pelvis and its ideal position can help us understand and correct postural mistakes during out daily activities.
This is especially important if we work out at a gym or do any kind of weightlifting.
Remember to breath normally though this exercise and do not hold your breath.

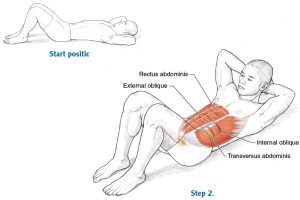
Chest Lift:
The chest lift is a beginner exercise that serves as foundation for more complex Pilates exercises.
Nonetheless, it is often performed incorrectly by many beginners that pull the neck up with their hands rather than performing a contraction of the abdomen.
This oftentimes leads to neck pain.
To correctly perform a chest lift, lay on the floor with your knees bent and your arms behind your head.
From this position, contract your abdomen slightly and gently lift your head off the floor.
Your arms are simply supporting your head but they are in no way pulling your neck.
The best way to remember the correct position is to lift your head as if trying to look at your belly button.
Remember to breathe!
Respiration is a crucial part of exercising.
If you hold your breath during this exercise you can trigger a sudden increase in blood pressure which could cause you to become dizzy and feel ill.
Swan Prep:
The Swan is a wonderful back exercise used in Pilates.
If performed correctly, the swan provides a great stretch for the lower back and chest.
Unfortunately, many people are not taught how to properly execute this exercise and it often creates irritation and pain while doing it.
As with most exercises, the Swan requires practice in order to improve the range of motion.
We often see photos or instructors performing this exercise and lifting their chest a great distance off the ground.
When you first start, it is unlikely your back will have the flexibility and capability of stretching this much.
Begin by lying face down.
From this position use your arms to gently lift your chest off the ground while keeping your legs flat on the ground.
Use your arms to lift your chest until you feel the stretch but no pain.
Your leg muscles should be relaxed and the motion comes from a stretch of your back.

Child’s Pose:
The child’s pose is often regarded as a resting pose in Yoga and Pilates.
This position is very comforting for those suffering from back pain.
Kneel on the ground resting your buttocks on your calves.
From this position, gently lean your chest forward towards the ground until your forehead touches the ground and slide your arms overhead.
You should feel a gentle stretch in your whole back.
If having your arms overhead is uncomfortable, you can rest them off to your sides.
Remember to breathe normally.

The exercises mentioned previously serve as an example of interventions using Pilates for back pain.
The best to find which exercises are the best for you and your back pain is to undergo a comprehensive evaluation.
This will determine the right progression needed and can avoid the use of exercises that will increase or worsen then symptoms.26
Are ready to incorporate customised for your needs Pilates exercises into your back rehabilitation program? Contact us now for a commitment free back pain consultation today clicking on this link HERE. Learn how personalised Pilates with a Rehabilitation Specialist can completely change your life.
What about Neck Pain?
We often thing of back pain when it comes to the lower back but neck pain is a pretty common symptom that relates to disability and work absenteeism.
It is estimated that 70%-80% of people suffer from neck pain at some time in their lives and up to 60% of the population may experience persistent and recurrent pain.27
Most often, neck pain is associated with:
- poor sleeping habits,
- poor posture,
- injury or physical trauma,
- stress
- anxiety and
- cervical radiculopathies.
Let’s review some of the main reasons why we struggle with neck pain.
Trauma
The cause of neck pain has many factors:
- inflammatory,
- degenerative changes
- postural changes adaptation or
- mechanical causes.
Important factors also include:
- bad alignment,
- low mood,
- neck strain, and
- sporting injuries.
Oftentimes, neck pain with decreased mobility is a common complaint after trauma.
Did you know that mechanical restriction and limited mobility between vertebrae can cause a decreased range of motion and stiffness may accompany neck pain?28
Neck trauma can be life threatening and lead to impairments if not treated properly.
Radiculopathies
Cervical radiculopathy refers to pain and/or sensory and motor deficit caused by compression of a cervical nerve root.
Neck pain and its related disability cause and important socioeconomic burden to society.7
Similar to lower back radiculopathies, the numbness and tingles of a cervical radiculopathy usually radiate to the arms.
Sleeping Habits
The type of pillow and mattress correlates to the appearance of neck pain.
A study explains that of all the different materials used for making pillows, latex pillows significantly decreased reports of waking cervical pain, and significantly improved sleep quality and pillow comfort scores.
Also, Polyester pillows were associated with significantly decreased reports of waking cervical spine stiffness.
Other pillow types did not significantly influence waking cervical symptoms.29
Postural Habits
Similar to lower back pain, prolonged postures of the head and neck can cause pain.
It has been commonly observed that patients who report with chronic pain in their neck often have associated forward head posture.
A forward head posture, also known as “hunched upper back”, is defined as anterior slanting of the neck over head in which the lower cervical spine goes into hyper flexion and the upper cervical spine into hyper extension associated with forwarding shoulders and rounded upper back.
The overload on the cervical spine resulting in fatigue of the neck muscles causes:
- pain,
- stiffness and
- other symptoms in the neck.30
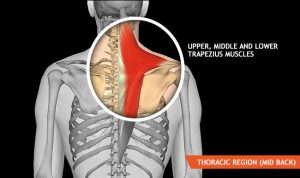
People with forward head posture presented weakness in several muscles including the scapular retractors (rhomboids, serratus anterior and middle and lower trapezius) and shortening or tightening of the cervical extensors or the pectoralis muscles.
To correct misalignment towards an ideal posture using a combination of strengthening, stretching, and postural training represent a significant component of the intervention.
Improvement in postural alignment secondary to exercise would be expected due to improvement in muscle length and/or strength.30
Conclusion:
Lower back pain and neck pain are extremely frequent conditions in people of all ages and nationalities.
These conditions are common reasons of work absenteeism and disability.
Trauma, posture and many other factors influence the appearance and disappearance of pain.
Although in many instances, the reason why pain appears is not a big concern and symptoms will usually subside in a few days with rest and over the counter pain killers, it is important to know the symptoms of other conditions that can create chronic back pain.
Customised exercise, proper postural habits and an extensive evaluation process can be key factors in decreasing and eventually eliminating back pain.
You don’t have to live life in pain!
A back rehabilitation specialist can guide you to living life to the fullest.
Book your Complete 12 Week Weight Loss Program If you have any questions or concerns about 12 weeks Body Transformation program, please contact jazz Alessi at: 020 3633 2299 (Monday – Fri: 6:30am to 9pm – Saturday: 8am to 3pm).
Request now a free consultation here https://www.personaltrainingmaster.co.uk/contactme/
For more information on back rehabilitation and injury rehabilitation services offered at our website, contact Jazz Alessi now.
References:
- Poquet, N., Lin, C.-W.C., Heymans, M.W., van Tulder, M.W., Esmail, R., Koes, B.W., Maher, C.G. Back schools for acute and subacute non-specific low-back pain. Cochrane Database of Systematic Reviews. https://doi.org/10.1002/14651858.CD008325.pub2
- Hurwitz, E.L., Randhawa, K., Yu, H., Côté, P., Haldeman, S. The Global Spine Care Initiative: a summary of the global burden of low back and neck pain studies. Eur Spine J 27, 796–801. https://doi.org/10.1007/s00586-017-5432-9
- Cohen, S.P., Hooten, W.M., 2017. Advances in the diagnosis and management of neck pain. BMJ j3221. https://doi.org/10.1136/bmj.j3221
- Costa, L. d. C.M., Maher, C.G., McAuley, J.H., Hancock, M.J., Herbert, R.D., Refshauge, K.M., Henschke, N., 2009. Prognosis for patients with chronic low back pain: inception cohort study. BMJ 339, b3829–b3829. https://doi.org/10.1136/bmj.b3829
- Maher, C., Underwood, M., Buchbinder, R., 2017. Non-specific low back pain. The Lancet 389, 736–747. https://doi.org/10.1016/S0140-6736(16)30970-9
- Kucharz, E.J., Mastalerz-Migas, A., Kwiatkowska, B., Gasik, R., Kotulska, A., Kowalczewski, J., Tomasik, T., 2016. Inflammatory low back pain: diagnostic and therapeutical recommendations for family doctors. fmpcr 3, 399–407. https://doi.org/10.5114/fmpcr/64779
- Parikh, J., 2017. Correlation of neck pain and disability in cervical radiculopathy. International Journal of Therapies and Rehabilitation Research 6, 223. https://doi.org/10.5455/ijtrr.000000269
- Verhagen, A.P., Downie, A., Popal, N., Maher, C., Koes, B.W., 2016. Red flags presented in current low back pain guidelines: a review. Eur Spine J 25, 2788–2802. https://doi.org/10.1007/s00586-016-4684-0
- Lucas, C., Costa, J., Paixão, J., Silva, F., Ribeiro, P., Rodrigues, A., 2018. Low Back Pain: A Pain That May Not Be Harmless. Eur J Case Rep Intern Med 5, 000834. https://doi.org/10.12890/2018_000834
- Fuso, F.A.F., Dias, A.L.N., Letaif, O.B., Cristante, A.F., Marcon, R.M., de Barros, T.E.P., 2013. Epidemiological study of cauda equina syndrome. Acta Ortop Bras 21, 159–162. https://doi.org/10.1590/S1413-78522013000300006
- Manusov, E.G., 2012. Low back pain.
- Osterhoudt, M., 2013. How to Ease Common Back Pain – Muscle Knots, Sciatica and Back Strain. Lulu Press, Inc.
- Ebnezar, J., 2012. Low back pain. Jaypee Brothers Medical Publishers (P) LTD, New Delhi.
- Weisman, M., 2010. Ankylosing Spondylitis. Oxford University Press.
- Tali, E.T., 2004. Spinal infections. European Journal of Radiology 50, 120–133. https://doi.org/10.1016/j.ejrad.2003.10.022
- National Collaborating Centre for Primary Care (UK). Low Back Pain: Early Management of Persistent Non-specific Low Back Pain [Internet]. London: Royal College of General Practitioners (UK); 2009 May. (NICE Clinical Guidelines, No. 88.) 2, Introduction. Available from: https://www.ncbi.nlm.nih.gov/books/NBK11709/
- Maniadakis, N., Gray, A., 2000. The economic burden of back pain in the UK. Pain 84, 95–103. https://doi.org/10.1016/s0304-3959(99)00187-6
- Gore, M., Sadosky, A., Stacey, B.R., Tai, K.-S., Leslie, D., 2012. The Burden of Chronic Low Back Pain: Clinical Comorbidities, Treatment Patterns, and Health Care Costs in Usual Care Settings. Spine 37, E668–E677. https://doi.org/10.1097/BRS.0b013e318241e5de
- Oliveira, C., Maher, C.G., Pinto, R., Traeger, A.C., Lin, CW.C., Chenot, J.F., van Tulder, M., Koes, B. Clinical practice guidelines for the management of non-specific low back pain in primary care: an updated overview. https://link.springer.com/article/10.1007%2Fs00586-018-5673-2
- Gregory, D.E., Dunk, N.M., Callaghan, J.P., 2006. Stability Ball Versus Office Chair: Comparison of Muscle Activation and Lumbar Spine Posture During Prolonged Sitting. Hum Factors 48, 142–153. https://doi.org/10.1518/001872006776412243
- Gordon, R.& Bloxham, S.; A Systematic Review of the Effects of Exercise and Physical Activity on Non-Specific Chronic Low Back Pain. https://www.mdpi.com/2227-9032/4/2/22/htm
- Statutory Register of Osteopaths; the GOsC Public Awareness Survey (2006) and the GOsC Osteopathic Practice Survey – Pilot Study (2006-07).
- Licciardone, J.C., Brimhall, A.K., King, L.N., 2005. Osteopathic manipulative treatment for low back pain: a systematic review and meta-analysis of randomized controlled trials. BMC Musculoskelet Disord 6, 43. https://doi.org/10.1186/1471-2474-6-43
- Clark, S. & Horton, R. Low back pain: a major global challenge. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(18)30480-X/fulltext
- Hayden, J., Cartwright, J., van Tulder, M.W., Malmivaara, A. Exercise therapy for chronic low back pain. https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD009790/full
- Yamato, T.P., Maher, C.G., Saragiotto, B.T., Hancock, M.J., Ostelo, R.W., Cabral, C.M., Menezes Costa, L.C., Costa, L.O., 2015. Pilates for low back pain. Cochrane Database of Systematic Reviews. https://doi.org/10.1002/14651858.CD010265.pub2
- Pawaria, S., Sudhan, D.S., Kalra, S., 2019. Effectiveness of Cervical Stabilisation Exercises on Respiratory Strength in Chronic Neck Pain Patients with Forward Head Posture- A Pilot Study. JCDR. https://doi.org/10.7860/JCDR/2019/39813.12777
- Yasin, M., Ijaz Gondal, M., Qamar, M., Basharat, A., Rasul, A., Ahmed, W., 2019. Effects of deep friction massage and static stretching in non-specific neck pain. Med J DY Patil Vidyapeeth 12, 331. https://doi.org/10.4103/mjdrdypu.mjdrdypu_196_18
- Gordon, S.J., Grimmer, K.A., Buttner, P., 2020. Pillow preferences of people with neck pain and known spinal degeneration: a pilot randomized controlled trial. Eur J Phys Rehabil Med 55. https://doi.org/10.23736/S1973-9087.19.05263-8
- Pawaria, S., Sudhan, D.S., Kalra, S., 2019. Effectiveness of Cervical Stabilisation Exercises on Respiratory Strength in Chronic Neck Pain Patients with Forward Head Posture- A Pilot Study. JCDR. https://doi.org/10.7860/JCDR/2019/39813.12777



