ACL Reconstruction Rehab Programme In London
What Are Your ACL Injury Rehab Goals?
- Do you want to achieve a successful knee rehab ?
- A sustainable weight loss after a knee surgery ?
- Learn how to stay in shape with a torn Anterior Cruciate Ligament ?
- Safely achieve your fitness goals with a rehabilitation personal trainer after ACL reconstruction surgery?
If you want to successfully achieve any of these goals, enjoy exercising with your family and friends or want a trustable, rehabilitation personal trainer after knee replacement you are in the right place.
Jazz Alessi is a long term specialised knee rehab professional and one of the best elite personal trainer in London.
He helps you with ACL graft healing, create for you personalised acl injury exercises to avoid re-injury, exercise and tailored diet plan to learning how to lose weight (increased BMI is a risk factor) with a torn anterior cruciate ligament and how to stay in shape after acl reconstruction surgery.
What are your main ACL targets and rehab goals?
Contact us now through this link.
Do you have a knee injury question you’d like it to be answered?
Contact us now through this link, HERE.
How to Successfully Rehab Your ACL Injury?
Your ACL reconstruction package is conveniently delivered at your London location whether this is your home, nearby park or office.
Jazz provides all the ACL rehab equipment, and you only need a space covering the size of a Pilates mat.
Jazz will work closely with your doctor, physiotherapist (if required) to getting you back fast and safe into optimum level of activities, exercise and competitive sport.
In order to understand the unique benefits of your personalised ACL reconstruction service please read below why we are known to deliver one of the very best and most effective ACL reconstruction rehab programme in London.
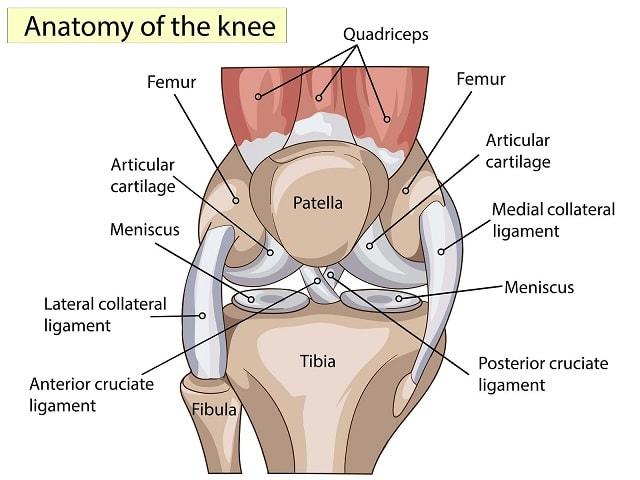
The four major knee ligaments are:
✓ Anterior Cruciate Ligament (ACL) located inside the knee joint controls back and forth movements
✓ Posterior Cruciate Ligament (PCL) located inside the knee joint is one of the cross ligaments (the other one is the ACL) controlling the forward and backwards movements
✓ Medial Collateral Ligament (MCL) located outside the knee joint stabilises, controls and limits knee sideway movements and protects it from hits and blows
✓ Lateral Collateral Ligament (LCL) located outside the knee joint controls, limits sideway movements and it stabilises the knee
The Medial and Lateral Collateral ligaments are present on either sides of the knee and control the sideways movement of the knee.
The Cruciate Ligaments
The Cruciate ligaments form the central pillar of the ligament complex of the knee joint.
They are short ligaments that run crisscross between the two articulating surfaces (femur and tibia), hence the name.3
They are responsible for the forward backward and rotational stability of the joint.
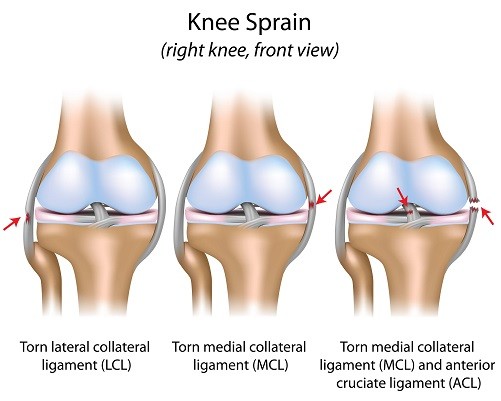
MCL Injury
The Medial Collateral Ligament is present on the inner side of the joint, and connects ends of tibia and femur.
This ligament is more prone to direct contact injuries (like football) as some of its fibres blend into the joint capsule making it rigid.
An inward thrust to the side of the knee with the foot firmly on the ground is the main mechanism of MCL injury.4
LCL Injury
On the other hand, the Lateral Collateral Ligament is present on the outer side of the knee, connecting the ends of femur and fibula.
It is more flexible and thus less likely to get injured. An outward thrust to the knee is the main mechanism of LCL injury.5
PCL Injury
The primary function of Posterior cruciate ligament (PCL) is resisting the backward glide of the tibia on the femur.
In addition, it also limits hyperextension and inward and outward rotation of tibia on the femur.
It is a much broader and stronger ligament as compared to the ACL and hence constitutes only 10% of the total knee injuries.
It is usually injured by a direct blow to the flexed knee resulting in excessive backwards sliding of the tibia (dashboard injury).
Excessive extension and rotational forces may also injure the PCL.3
“My ACL injury rehabilitation program was fully customised. Any exercise I couldn’t perform was changed. When I started, I had no flexibility, balance and I felt lots of pain in my knee. Once I started training with Jazz I immediately felt a big improvement. I also saw an increased in strength, flexibility, body coordination, exercise flow and I could do more exercises then as I could when I started.
As time went on the pain dramatically reduced.
I 100% recommend Jazz Alessi injury rehabilitation services.”
– Aaron Cadette –
Would you like to get rid of your knee pain, and successfully rehabilitate your ACL injury?
Contact us now through this link, HERE.
How Your ACL Ligament Gets Injured
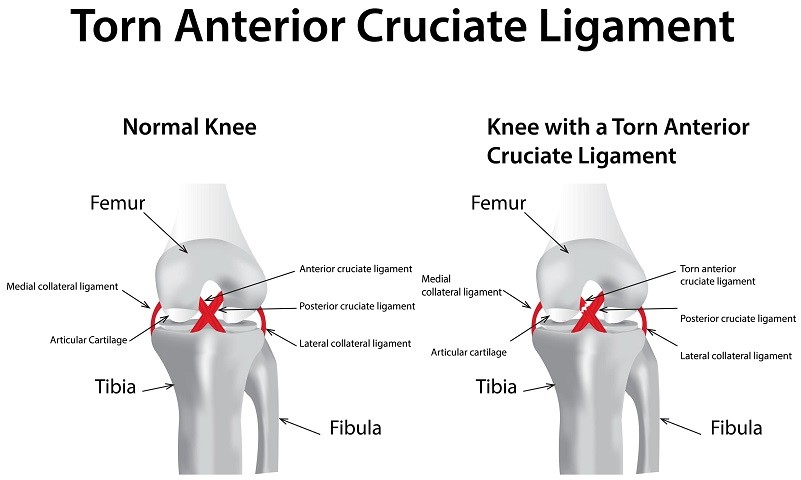
The Anterior Cruciate Ligament (ACL) acts as the anterior restraint (prevents the forward glide of tibia on femur) to the tibia during flexion and extension of the knee joint.
It also acts as a rotatory restraint to inward rotation of tibia during knee flexion.
The most common mechanism of injury is the rapid deceleration and sudden cutting movement with foot firmly planted on the ground (also known as cut and plant motion).1
Causes of ACL injury:
ACL injury is one of the commonest ligament injuries in many of the fast-paced games.
There are many factors responsible.
1 Shoe- surface interface. Evidence dictates that risk of ACL injury is 2.5 times higher when there is more rotational traction at the shoe-surface interface.
Though some amount of friction improves sports performance, it can also increase the risk of ACL injury.
The edge design of cleats (irregular long cleats in the periphery and short regular cleats in the interior) have been associated with highest percentage of ACL injuries.6
2 Age: 70% of ACL injuries are non-contact injuries in athletes between 15-45 years of age.1
Younger individuals are more prone as they are more involved in competitive sports with pivoting, decelerating and jumping actions.1
Age associated ligament laxity and skeletal immaturity can be the probable causes.1
3 Gender: Women are 2-8 times more prone to ACL injury than men in same sports due to gender related differences in loading mechanisms and joint geometries and neuromuscular control in the trunk, pelvis and hip.8,9
4 Reduced core stability has also been seen as an important cause of ACL injury.
Weakness in the abdominals, hip abductors and external rotators causes pelvic to tilt forwards.
It also increases inward rotation of the femur, that places increased inward stress on the knee.
This, doubles the risk of ACL injury. 10
5 Previous history of ACL injury disturbs the normal loading and muscle activity around the injured as well as uninjured knee, making it prone to injury.11
6 Position of the leg for example excessively straight knee with directed inwards places greatest stress on the ACL ligament.12
Another triggering position is when the athlete attempts to change direction suddenly on an inwardly deviated and flexed knee.14
7 Dry weather: It has been noted that non-contact ACL injuries in football were more common during periods of low rainfall and high evaporation.13
8 Neuromuscular control – Poor muscle control around the hip, knee and ankle have been increasingly implicated in the injury of ACL.15
ACL Injury and Effects on Lower Body Stability and Coordination Tend to Escalate Rapidly, Research Says
Injury to the ACL is regarded as very serious as it affects the kinematics of the knee joint causing long term complications.
It has been reported that the initial trauma and resultant changes may cause meniscal and cartilage damage and degenerative changes leading to early onset OA (osteoarthritis).16
In addition to forward restraint, the ACL also acts as a restraint to inward rotation of tibia during knee flexion.
These rolling and gliding motions between the surfaces allow for full flexion and extension of the joint.
The shallow and incongruent articular surfaces are unable to provide the necessary stabilisation in weight bearing positons for these subtle movements.
The cruciate ligaments along with the menisci and muscles are accountable for the functional range of movement (ROM) and joint stability in standing, running, walking etc.1
The complex knee motion recruits all the 4 major ligaments in various combinations to provide stability as the knee bends.17
The ACL provides more than 80% of restraint between 30-90 degrees of knee flexion.
It also restrains excessive inward rotation of tibia during extension.18
Injury to the ACL thus impacts the knee function by affecting the dynamic stability.
The sensory receptors in the ligament send feedback about the position of the joint (proprioception).
This feedback reduces after injury.
The feedback from knee governs the muscle coordination between the hip and ankle during running, cutting etc.
This in turn affects the knee position and increases the chances of a second ACL injury.19
Dynamic stability of the knee is dependent on accurate sensory input and appropriate motor responses to rapid changes in body position during cutting and landing. 20,24
Neuromuscular control of the hip, trunk, and knee is based on feedback control.
The position of each segment affects the position of segment below.11
Poor feedback from the knee, impairs the trunk control further enhancing the risk of ACL injury. 29
When are not rehabbed, knee injury create many types of compensatory mechanisms changing your movement biomechanics, muscle unitisation and tend to cause much bigger problems escalating rapidly.
Thus, during the examination of a suspected ACL injury, mechanism of injury becomes crucial.
Would you like to get rid of your knee pain, and successfully rehabilitate your ACL injury?
Contact us now through this link, HERE.
How Your Sport Medical Doctor Evaluates an ACL injury

The ACL is the most frequently injured structure in the knee with more than 70% cases resulting due to non-contact injuries where the foot is firmly planted on the ground and the athlete changes direction suddenly.
Direct contact injuries are seen in tackle sports such as football.
The client or the athlete may also report of severe pain and an audible pop or crack at the time of injury with episodes of giving way while running or pivoting.
He may also complain of instability.
There may be visible swelling.
Knee extension may be painful and limited.
There are reliable specific tests help to identify the ligament involved.
The Pivot shift test (rotatory instability) and the Lachman test (forward back ward instability) are more accurate in detecting a subacute or chronic ACL tear as compared to the routine anterior drawer test (forward back ward instability). 20
How Grade 1, 2 and 3 Knee Sprains Will Affect Your Knee Recovery
Depending on the symptoms, the ACL tear is graded as below:
Grade 1 sprain: The ligament fibres are stretched with no actual tear.
There is mild tenderness and swelling with no feeling of instability or giving way.
There is a firm end feel with no ligament laxity elicited while testing.
Grade 2 sprains: The ligament fibres are partially torn with haemorrhage.
There is tenderness and swelling around the knee with noticeable loss in function due to pain.
Ligament laxity with firm end feel is noted while testing.
The athlete reports of episodes of giving way or instability during activity.
Grade 3 sprains: There is complete breach of ligament integrity.
The knee is unstable with more episodes of giving way.
There is tenderness and moderate swelling but less pain.
There is rotational instability with no firm end point.
This is also referred to as an ACL deficient knee which needs ligament reconstruction to return to activity.
Would you like to get rid of your knee pain, and successfully rehabilitate your ACL injury?
Contact us now through this link, HERE.
Why Your ACL Injury Affects Other Ligaments and Knee Muscles and How to Avoid This Before Is To Late
ACL injuries rarely occur alone.
When occurring along with MCL and Medial meniscus injury, it is called as an Unhappy Triad or O’Donoghue triad.
There may be a very small injury to the subchondral bone, cartilage, tibial surface etc.
In some cases, there may also be associated injuries to the lateral collateral ligament, the posterior capsule and the popliteus muscle and tendon.
These are more evident on X-rays or MRI.
Since your body weight relies on healthy legs and the ACL injury has the ability to affect both positively and negatively your life forever, the knee rehabilitation is a very serious matter.
After a full screening of the knee joint it is important to assess the functional status of the patient, lifestyle, risks and his quality of life.
These and other very important elements will help us to set effective rehab goals for you and decide the very fine personalisation approach according with your particular needs, knee rehabilitation phases as well as the progression or regression of exercises.
The Knee Injury and Osteoarthritis Outcome Score (KOOS) questionnaire also evaluates the functional status and quality of life (QoL) of patients with any type of knee injury who are at increased risk of developing OA; i.e., patients with anterior cruciate ligament (ACL) injury, meniscus injury, or chondral injury.22
It has been proven that patient based outcome measures give a better picture of the quality of life than clinical tests alone.
Risk Factors for ACL Injuries
There are certain factors that up the risk of ACL injury.
- Contact and pivoting sports –The pivoting action in sports like football and basketball or recreational plays where the client or the athlete swerves suddenly to avoid collision with another player is the main mechanism of injury.
The foot is planted on the ground and sudden change of direction provides an inward thrust on the bent knee.
This is a typical non-contact deceleration injury. 23
- Poor joint position sense and proprioception does not elicit timely recruitment of the quadriceps and the hamstring muscles.
The weak hip and ankle coordination and the low pelvic- hip control (core stability) as a result of poor core stability is another factor for recurrent ACL injury. 25
- Incorrect landing techniques for example landing with less knee flexion or greater inward deviation (Position of No Return), places greater stress on the ACL. 25
- Active contraction of quadriceps (reflective eccentric contraction) during jump stop landings in athletes with weaker hamstrings puts more load on the ACL causing it to rupture.1
- Foot hyperpronation: Athletes with increased foot pronation and internal tibial rotation usually have a greater anterior knee joint laxity which puts the ACL at increased risk of injury. 24
- Fatigue and Loss of concentration – compound the existing compromised neuromuscular control thus increasing the chances of ACL injury. 1
- Anatomic differences in men and women – Difference in the knee joint geometries and generalised ligament laxity make an athlete especially females more prone to ACL injuries. 25
It is hypothesised that increased bone length and body mass, in the absence of matching adaptations in neuromuscular strength and coordinated muscle recruitment, expose the female knee to greater load and likelihood of ACL.30,31,12,16,32
Females are also more prone to ACL injuries in the pre-ovulatory phase.
Estrogen has also been linked to increased risk of ACL damage in females.
- Increased BMI and inactive lifestyle – Increased body weight in the presence of abnormal knee joint geometries can put increased loads on the knee as well as the ACL ligament raising the risk of injury. 26
Younger individuals are at more risk of ACL injury due to their highly active lifestyle.
Recurrence of injury may be noted when individuals return too early to exercising, competitive sports or high activity games after a conservative rehab program.
Individuals who practice moderately active lifestyle (reduced frequency and intensity of exercise).28
On the other hand, those individuals who opted a sedentary lifestyle due to re-injury fears led a low quotient of happiness and poor quality of life. 28
- Competition versus Practice – ACL injuries are more likely to occur in competition as opposed to practice matches.
This may be due to the increased aggression during matches. 40
Consequences of ACL Injury on The Gait, Alignment and Foot
Client with ACL compromised knee joint, present with quadriceps, hip muscles and calf weakness and increased activation in the hamstrings. 35, 37 This results in impaired hip – ankle coordination while walking due to incorrect feedback from the knee.19 These clients also exhibit weakness in the hip abductors and external rotators. This results in weakness of the major core muscle – multifidus. The resultant pelvic tilt and trunk sway causes further medial knee collapse and re-injury to the ACL. 33 Weakness of the multifidus resulted in chronic back pain in many individuals with ACL deficient knee. ACL deficiency also causes increased tibial inward rotation and flattening of the medial foot arches. 34
We are all different.
I will professionally work with you and successfully help you addressing all your injury specific technicalities to reduce, retrain and eliminate the negative conseqeances you your knee injury.
What is an ACL Rehab Program and How does it help?
An ACL rehabilitation protocol is a scientifically designed exercise plan which helps the client to return to optimum functional status within a span of 4-9 months.
An athlete who wishes to return to highly competitive sports will need around 12 months of rehabilitation. 36
We will also show you how to lose weight with a torn acl and in a safe manner how to stay in shape with a torn ACL.

We will take you successfully through all rehabilitation phases and teach you how to enjoy running again and how to stay in shape after knee surgery – in a safe way.
The knee rehabilitation programme varies depending on the extent of ACL injury (grading) and includes specific techniques to (but, not limited to) switching off overactive muscle, activating dormant muscles, carefully designed stretches, addressing postural problems, neuro training, compensatory movements, personalised knee strengthening exercises and many other modules we use to ensure your ACL rehab is successful.
Although there are some commonalities the knee strengthening exercises and the whole rehab approach for runners will be very different from an MMA fighter, wrestles, tennis player, skiing or a bodybuilding.
It also depends whether the rehab it is being done after ACL reconstruction or is being done to avoid surgery thus, it is essential to work with a long term rehabilitation coach personal trainer after acl surgery to achieve a successful rehab.
The rehab protocol is divided into personalised phases and the progression (intensity, frequency and complexity of exercise).
The progression to the next stage happens when the knee shows no signs of pain and inflammation with the exercises of the previous phase.
According to the clinical practice guidelines laid by APTA for knee ligament injuries, intervention strategies are based on timeline after the injury. 36
The immediate and early rehabilitation strategies focus on reducing the pain and swelling, and immobilising the knee for a period of 1 week.
This phase also emphasises achieving full ROM at the knee with special attention to knee extension.
The neuromuscular stimulation helps to maintain the strength in the quadriceps and hamstring which prevents deconditioning.36
We encourage the clients to work safe and mobilise early to improve normal muscle contraction, enhance proprioception and normalise walking pattern.
The later phase of rehabilitation has more functional strategies that work towards improving lower extremity muscle strength and flexibility bilaterally through therapeutic exercises.
More OKC (open kinetic chain) and CKC (open kinetic chain) exercises are begun to improve stability and functional strength around the knee.
These should be started around 4-6 weeks after injury/surgery and continued for next 6 months thus, is why is essential to have all rehab supervised and work with a long term elite personal trainer after acl surgery.
The phase also includes neuromuscular re-education to improve muscle activation, balance, coordination, core stability and correct movement impairment in the lower extremity (hip-knee-ankle).
One of the goal of this phase is to reduce the episodes of ‘giving way.’
When the knee exercise drills aren’t personalised the client risk re-injury however, one to one personal training after knee surgery eliminates re-injury risk.
The supervised rehabilitation phase under close supervision with an elite personal trainer after acl surgery takes the client and the athlete preparing it appropriately for on field activities including personalised agility drills that involve sudden start and stop, cutting, running etc.
The movement of the neck, spine, shoulders, arms, trunk, hip and knee and ankle are carefully monitored to identify the form, bio mechanical power transfer faults, compensatory movements etc, and correct them on the spot to avoid re-injury whilst, maximise the knee rehabilitation effectiveness.
Field tests like hop tests (6 metre timed hop test, crossover hop test for distance, triple hop test for distance and single hop for distance) could test the athlete’s neuromuscular control, movement symmetries, overall knee function and return to sports. They can also help to form the baseline for the next stage and set of exercises.
In the last phase of rehab, the athlete’s physical and psychological readiness to return to sports or normal function is tested.
The client based outcome measure/questionnaires help to evaluate the readiness and progress throughout the intervention.
Based on the outcome a reconstruction surgery can be advised or activity modification can be suggested.
Having an injury rehabilitation coach and the best personal trainer in London on your side really helps in such cases since clients are 30% more likely to achieve their targets when they are working under supervision.
Supervised rehab personal training also helps you to avoid knee re-injury.
Since the rehabilitation elite trainer is in sync with the patient’s thoughts and emotions, he is the best person to supervise the exercise form, implement the unique approach and to check the client from underdoing or overdoing any exercise.
The sports rehabilitation trainer has a lot of accurate professional tools in his armoury.
In-depth knowledge of exercise physiology, nutrition and sports psychology improve muscle performance, tissue health and instilling confidence.
All these factors in combination help to improve mental strength, knee function and movement strategies.
This in turn improves the patient’s quality of life and enables her/him in getting back to optimum activities or on the field as soon as possible.
Would you like to get rid of your knee pain, and successfully rehabilitate your ACL injury?
Contact us now through this link, HERE.
What Type of Nutrition Helps You To Lower Inflammation, Pain Levels and Improve Mental Focus
Food items could upregulate or downregulate pain levels.
Sugar and process foods could upregulate pain levels.
It has been proposed that consumption of some foodstuffs can enhance healing and reduce inflammation.
Foods rich in Omega 3, Glucosamine chondroitin complex with M&M and antioxidant rich foods (food with Vitamin C and E) have been associated with reduced pain and inflammation and faster healing.
They have also showed energy building, weight loss, improved mental health and anti-ageing properties as they slow the degenerative process.
Turmeric, bromelain and garlic are just a few foods which have been known to contain anti-inflammatory properties.
The American Dietetic Association recommends eating foods with low saturated fat but high nutrient content.
Spinach, turnips and mangoes are rich in vitamin A, important for cell growth.
Kiwis, cabbage, baked sweet potatoes, tomatoes, and cantaloupe offer non-citrus alternatives for vitamin C.
Almonds have a high zinc content, which aids in wound healing. 38,39
If is required Jazz will design for you an easy to follow healthy nutrition diet plan to helps you to lower inflammation levels, reduce pains, lose weight fast and safe, increase energy levels, improve your mood, skin texture and to reduce the effect of ageing.
Benefits of an ACL Rehab Program
A scientifically drafted customised ACL rehab programme will effectively speed up the recovery of any individual with ACL injury.
Since your knee is sensitive this will help you to avoing any knee re-injury risks.
ACL rehab program can be specifically designed for someone recovering from grade 1or 2 ACL sprains or someone who wishes to avoid surgery or for someone who wishes to return to optimum movement, exercise, competitive sports after a reconstruction surgery.
The incidence of a knee flexion contracture is associated with quadriceps weakness and extensor mechanism dysfunction.1
The ACL rehab program avoids this by encouraging early weight bearing, ROM exercises, quadriceps strengthening, switching off overactive muscles, activating the right muscles, skill based exercise, correcting compensatory movements but, not limited to.

Guidance on developing strength and neuromuscular control in bilateral lower extremities and the core ensures a much faster recovery.
Introduction of personalised and complex exercises challenges push the client and athlete to work harder in each progressive phase and also fills him/her up with positive emotions.
Among other things this helps the client to overcome fear of instability.
The ACL rehab program more importantly addresses the issue of prevention of re-injury by correcting the whole or part of the technique.
Also, the closed kinematic chain exercises stimulate coordinated muscle work around the knee reducing the shear force between the knee joint surfaces.
This reduces the stress on the ACL playing a vital role in preventing recurrence of injury.1
The knee rehabilitation programme also emphasises on maintaining and improving the cardiovascular endurance through customised cross training strategies.
This professional service also teaches you how to stay in shape after knee surgery and how to lose weight with a torn acl thus, working safe with an elite personal trainer after ACL surgery benefits you beyond the knee rehab.
The ACL knee rehab also works on the exercise enthusiast or athlete’s ability to focus and deal with distractions in the form of on negative street events, field perturbations or opponents.
During this phase, the client or the athlete is counselled on his ability to return to regular exercise or competitive training and professional guidance in terms of planning his/her competition year.
The client/athlete is guided on how to space major events like charity runs, marathon, triathlon, tough mudder, skiing competitions etc, or tournaments with some minor matches and rest periods to prevent recurrence.
The knee rehab also addresses any coexisting ligament or meniscal injuries which may be inhibiting full recovery.
The ACL rehab is futuristic as the athlete also gets advice on any exercise and activity modification that may be needed to stall the development of early onset arthritis.
Would you like to rehabilitate your ACL injury, to feeling again at your best ?
Contact us now through this link, HERE.
Personalised ACL injury Rehab Programmes by Jazz Alessi
Coming back from an ACL injury can be frustrating especially when the client or the athlete is at the top of their physical form.
The urge to hasten the rehab and overdo the exercises must be supervised and checked by a personal trainer after acl surgery as it will only delay the recovery by months whilst increasing dramatically the re-injury risks and a negative rehab outcome.
As a professional service provider of personal training after knee surgery with special interest in ACL knee rehab and an elite personal trainer, I understand what an ACL deficient knee needs.
Since more than 10 years, I have been rehabilitating around 20 – 30 people with acute and chronic knee injuries (ACL, PCL and Meniscus), each year on a one to one basis.
Using cutting edge technology, latest investigative tools and comprehensive assessment can help you to get an accurate picture of your injury.
I believe in working closely with your physiotherapist and sport medical doctor to conduct a thorough diagnostics and risk assessment before creating personalised and effective rehab plans for you.
This scientifically formulated knee injury rehab plan is tailor made for each individual and if required I will liaise with your physiotherapist and sport medical doctor.
As I deal with a variety of clients on and off the field, I understand the stresses put on the knee in various type of movements, sports and occupations.
My expertise in body mechanics and physiology is an important skill set, as this helps me understand the functional expectations of my clients.
As an injury rehabilitation trained elite personal trainer, and 2nd Generation Pilates teacher I understand how a body as a whole, responds to ACL injury.
I focus on understanding the client’s current needs, fitness levels prior to the injury, his movements, lifestyle, game style (if the client is an athlete), biomechanical variations in the knee and the entire lower and upper extremity and his expectations after the ACL tear.
Each rehab case is different; some clients may have an isolated ACL tear while others may have other concomitant injuries to the meniscus or other ligament or other type of knee imbalances.
My ACL rehab programme covers all these issues.
I use a multidimensional approach in the management of ACL injuries, combining effective and personalised ACL rehab exercises but, also selected body conditioning, Pilates, Yoga, gymnastics, martial arts and weights to get the best results whilst keeping your training very entertaining.
As a 2nd generation Pilates trainer, I use advanced biomechanics and knowledge of the core to design a preventive rehab for ACL injury cases.
A personalised nutrition diet plan will improve your energy levels, performance, and skin, enhance healing and prevent ageing and joint degeneration.
All these play an important role in returning to optimum movements, better mental health and achieving peak performance.
My clients are banking executives, CEO’s, lawyers, doctors, actresses and actors, marathon runners, Olympic athletes and footballers who enjoy my entertaining sessions as they get a complete rehab package when it comes to their ACL injury rehab.
I also focus in working with the client physical structure as a whole, rather than the joint alone.
Your personalised rehab package is very effective, fun, challenging and goal oriented.
All knee injuries rehabilitation packages are provided in Canary Wharf, Kensington, Central London, North London, whilst I am covering all Greater London and I am very flexible with time.
If you are suffering from an ACL injury wish to get rid of pain, regain your optimum movement for day to day living and peak performance, you can contact me on now by clicking on this link HERE, and I will get back to you.
REFERENCES:
- J. Dargel, M. Gotter, K. Mader, D. Pennig, J. Koebke, R. Schmidt-Wiethoff “Biomechanics of the anterior cruciate ligament and implications for surgical reconstruction”. Strategies in Trauma and Limb Reconstruction,2007 April;Volume 2, Issue 1, pp1–12
- Physiopedia – Posterior Cruciate Ligament
- Physiopedia – Anterior Cruciate Ligament (ACL) Injury
- Physiopedia – Medial Collateral Cruciate Ligament Injury of the Knee
- Physiopedia – Lateral Collateral Cruciate Ligament Injury of the Knee https://www.physiopedia.com/Lateral_Collateral_Ligament_Injury_of_the_Knee
- Lambson RB, Barnhill BS, Higgins RW “Football Cleat Design and Its Effect on Anterior Cruciate Ligament Injuries: A Three-Year Prospective Study” American College of Sports Medicine, 1996, March 1; 24 (2): 155-159 https://doi.org/10.1177/036354659602400206
- Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD “Risk of Secondary Injury in Younger Athletes After Anterior Cruciate Ligament Reconstruction” Am J Sports Med. 2016 Jul; 44(7): 1861–1876. doi: 10.1177/0363546515621554. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC550124
8. Hewett TE, Myer GD, Ford KR, Powers S. “Book: Neuromuscular Intervention Targeted to Mechanisms of ACL Load in Female Athletes” National Institutes of Health; 2008.
- Hewett TE, Ford KR, Myer GD, Wanstrath K, Scheper M. “Gender differences in hip adduction motion and torque during a single leg agility maneuver” J. Orthop. Res. 2006; 24:416–421. https://www.ncbi.nlm.nih.gov/pubmed/16479597
- LEETUN D. T, IRELAND KL, WILLSON JD, BALLANTYNE BT, DAVIS IM “Core Stability Measures as Risk Factors for Lower Extremity Injury in Athletes”. Med. Sci. Sports Exerc., 2004 36(6), pp. 926–934,
- Pollard CD, Stearns KM, Hayes AT, Heiderscheit BC “Altered Lower Extremity Movement Variability in Female Soccer Players During Side-Step Cutting After Anterior Cruciate Ligament Reconstruction.” AJSM Vol: 43(2):460-465
- Brukner, Khan. Clinical Sports Medicine. 3rd edition. Ch 27.Tata McGraw- Hill Publishing. New Delhi.)
13. John Orchard, Hugh Seward, Jeanne McGivern “Intrinsic and Extrinsic Risk Factors for Anterior Cruciate Ligament Injury in Australian Footballers.” AJSM 2001, 29(2): 196-200
- Olsen OE, Myklebust G, Engebretsen L, et al. “Injury mechanisms for anterior cruciate ligament injuries in team handball: a systematic video analysis. Am J Sport Med 2004;32(4):1002-12.
- Sugimoto D. et al. “Compliance With Neuromuscular Training and Anterior Cruciate Ligament Injury Risk Reduction in Female Athletes: A Meta-Analysis” J Athl Train, 2012; 47(6): 714-723.
16. Kaeding CC, Pedroza AD, et al “Risk Factors and Predictors of Subsequent ACL Injury in Either Knee After ACL Reconstruction The American Journal of Sports Medicine, 2015 Apr 21; 43 (7): 1583-1590.
17. Muller W “The knee: form, function, and ligament reconstruction”
18. Butler DL, Noyes FR, Grood ES “Ligamentous restraints to anterior-posterior drawer in the human knee. A biomechanical study” J Bone Joint Surg Am, 1980 Mar;62(2):259-70.
- Paterno MV, Kiefer AW et al “Deficits in Hip-Ankle Coordination in Female Athletes who Suffer a Second Anterior Cruciate Ligament (ACL) Injury after ACL Reconstruction and Return to Sport” The Orthopaedic Journal of Sports Medicine, 2014; 2(7)(suppl 2)
- Katz JW, Fingeroth RJ “The diagnostic accuracy of ruptures of the anterior cruciate ligament comparing the Lachman test, the anterior drawer sign, and the pivot shift test in acute and chronic knee injuries” The American Journal of Sports Medicine 1986;14:88-91.fckLR (accessed 18 July 2013).
- William E.Prentice, Rehabilitation techniques for sports medicine and athletic training; fourth ed. McGraw Hill publications.
- E. Carlos Rodriguez-Merchan “Knee instruments and rating scales designed to measure outcomes” J Orthop Traumatol, 2012 Mar; 13(1): 1–6. Published online 2012 Jan 25. doi: 10.1007/s10195-011-0177-4
- Bing Yu and William E Garrett “Mechanisms of non‐contact ACL injuries” Br J Sports Med. 2007 Aug; 41(Suppl 1): i47–i51.
- Becky Woodford-Rogers, Lynne Cyphert,Craig R. Denegar, “Risk Factors for Anterior Cruciate Ligament Injury in High School and College Athletes” J Athl Train. 1994 Dec; 29(4): 343–346. PMCID: PMC1317810
- Helen C. Smith, Pamela Vacek, Robert J. Johnson, James R. Slauterbeck, Javad Hashemi, Sandra Shultz, and Bruce D. Beynnon, “Risk Factors for Anterior Cruciate Ligament Injury :A Review of the Literature — Part 1: Neuromuscular and Anatomic Risk” Sports Health. 2012 Jan; 4(1): 69–78. doi: 10.1177/1941738111428281
- Katherine M. Bojicic, Melanie L. Beaulieu, Daniel Imaizumi Krieger, James A. Ashton-Miller, Edward M. Wojtys, “Body Mass Index, Modulated by Lateral Posterior Tibial Slope, Predicts ACL Injury Risk” Orthop J Sports Med. 2016 Jul; 4(7 suppl4): 2325967116S00129. Published online 2016 Jul 29. doi: 10.1177/2325967116S00129
27. https://www.everydayhealth.com/acl-tear/guide/
28. https://www.sciencedirect.com/science/article/pii/S1836955316000205
- Hurd WJ, Chmielewski TL, Snyder-Mackler L. “Perturbation-enhanced neuromuscular training alters muscle activity in female athletes” Knee Surg. Sports Traumatol. Arthrosc, 2006;14:60–69.
- Krosshaug T, Nakamae A, Boden BP, et al. “Mechanisms of anterior cruciate ligament injury in basketball: video analysis of 39 cases” Am. J. Sports Med. 2007;35:359–367.
- Hewett TE, Myer GD, Ford KR, Powers S. Book Neuromuscular Intervention Targeted to Mechanisms of ACL Load in Female Athletes. National Institutes of Health; 2008. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4168968/
- Lauren E. Imwalle,1,2 Gregory D. Myer,1,3 Kevin R. Ford,1,2 and Timothy E. Hewett1,2 “Relationship Between Hip and Knee Kinematics In Athletic Women During Cutting Maneuvers: A Possible Link to Noncontact Anterior Cruciate Ligament Injury and Prevention”, J Strength Cond Res. 2009 Nov; 23(8): 2223–2230.
- Hwang-Bo Kak, Sun-Ja Park, Byun-Joon Park, “The effect of hip abductor exercise on muscle strength and trunk stability after an injury of the lower extremities” . J Phys Ther Sci, 2016 Mar; 28(3): 932–935. Published online 2016 Mar 31. doi: 10.1589/jpts.28.932
- Beckett ME, et al. “Incidence of hyperpronation in the ACL injured knee: a clinical perspective.” J Athl Train, 1992;27:58-62
- Yohei Shimokochi, Sae Yong Lee, Sandra J Shultz, Randy J Schmitz, “The Relationships Among Sagittal-Plane Lower Extremity Moments: Implications for Landing Strategy in Anterior Cruciate Ligament Injury Prevention” J Athl Train. 2009 Jan-Feb; 44(1): 33–38. doi: 10.4085/1062-6050-44.1.33
- David S. Logerstedt, Lynn Snyder-Mackler, Richard C. Ritter, Michael J. Axe, Joseph J. Godges, “Knee Stability and Movement Coordination Impairments: Knee Ligament Sprain Clinical Practice Guidelines Linked to the International Classification of Functioning, Disability, and Health from the Orthopaedic Section of the American Physical Therapy Association” J Orthop Sports Phys Ther. 2010 Apr; 40(4): A1–A37. doi: 10.2519/jospt.2010.0303
- Thomas AC1, Villwock M, Wojtys EM, Palmieri-Smith RM“Lower extremity muscle strength after anterior cruciate ligament injury and reconstruction.” J Athl Train. 2013 Sep-Oct;48(5):610-20. doi: 10.4085/1062-6050-48.3.23.
- https://www.health.harvard.edu/staying-healthy/foods-that-fight-inflammation
- Matthew C.Fadusa, Cecilia Laub, JaiBikhchandanic, Henry T.Lynchc “Curcumin: An age-old anti-inflammatory and anti-neoplastic agent” Journal of Traditional and Complementary Medicine. July 2017, 7( 3) :339-346
- Allan M. Joseph, Christy L. Collins, Natalie M. Henke, Ellen E. Yard, Sarah K. Fields, R. Dawn Comstock, “A Multisport Epidemiologic Comparison of Anterior Cruciate Ligament Injuries in High School Athletics.” J Athl Train. 2013 Nov-Dec; 48(6): 810–817.